
A new piece on NPR suggests that it’s okay to risk a baby’s death in order to bed share.
The piece asks Is Sleeping With Your Baby As Dangerous As Doctors Say? and answers by suggesting that the “right” kind of parents can bed share while the “wrong” kind of parents cannot.
[pullquote align=”right” cite=”” link=”” color=”” class=”” size=””]Is the relative risk irrelevant? Is it only the absolute risk that counts? Who gets to decide?[/pullquote]
Parents who drink or do drugs shouldn’t be sleeping with their babies because they could roll over onto their child. Babies who are born premature or whose parents smoke shouldn’t sleep in the parents’ bed because of potential respiratory problems. Suffocation can also happen when babies sleep on sofas because babies can be trapped between a parent and the cushions…
But what about the “right” kind of parents?
So far, only two studies have looked at this question. And doctors and families need to be careful with how they interpret these studies, says Robert Platt, a biostatistician at McGill University, who analyzed the studies for the AAP.
“The evidence is quite thin or weak,” he says. In both studies, the number of SIDS cases is small. One study of 400 SIDS had 24 cases in which that baby had shared the bed in the absence of parental hazards, and in the other study, there were just 12 of these cases out 1,472 SIDS deaths. In the latter study, some information about the parent’s drinking habits was missing and had to be estimated.
Nevertheless, the two studies came to similar conclusions. For babies older than 3 months of age, there was no detectable increased risk of SIDS among families that practiced bed-sharing, in the absence of other hazards.
Nevertheless? Pro-tip for the folks at NPR: when a study is underpowered, the results are not valid. You cannot use them to make recommendations. But let’s imagine for the moment that these statistics are accurate.
Even the “right” parents can still smother an infant less than 3 months old.
And for babies younger than 3 months?
“I would probably say there may be an increased for this group,” Platt says. “And if there is an increased risk, it’s probably not of comparable magnitude to some of these other risk factors,” such as smoking and drinking alcohol.
NPR includes a chart that attempts to distinguish when it’s okay to risk a baby’s death from when it’s not.
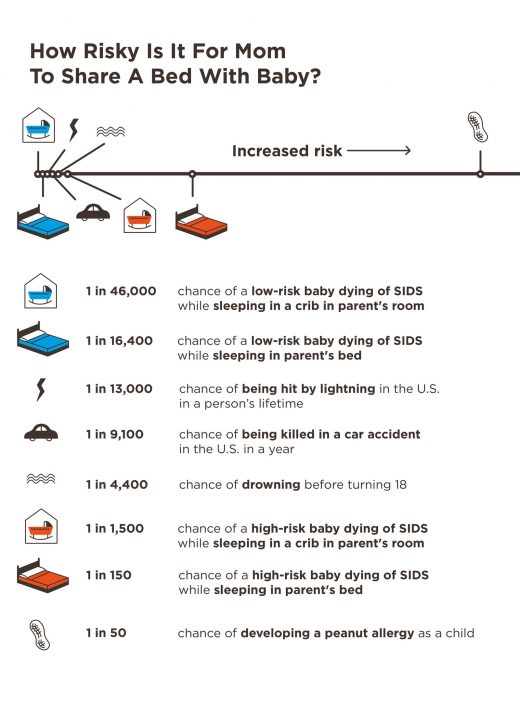
The chart implies that tripling the risk of a baby’s death by bed sharing in the “right” situation is acceptable because the absolute risk is low — 1 in 16,4000. In other words, it purportedly doesn’t matter how much a particular maternal action increases the risk of death as long as the absolute risk is low.
Is that what we really believe?
Consider the case of infants and car seats. According to the Insurance Institute for Highway Safety, from 1975 to 2013, infant fatalities fell from 6/100,000 (1 in 16,7000) to 1.3/100,000 (1 in 76,900) while car seat use rose to 99% of children under age 1. So the risk of death from to a baby riding in a car without a car seat is LOWER than the risk of death from bed sharing.
If it’s the absolute risk that counts and not the increase in relative risk than mothers who don’t strap their babies into car seats are better mothers than those who bed share, right? If it’s only the absolute risk that counts — as implied by breastfeeding researchers — that’s the inevitable conclusion.
How about formula feeding? Breastfeeding decreases the risk of SIDS, but the absolute risk is low in any case. Bed sharing when parents do not smoke: is there a risk of SIDS? An individual level analysis of five major case–control studies was referenced by Dr. Platt above.
Here’s a chart from the study:

Notice that the absolute risk of SIDS from formula feeding without bed sharing is LOWER that the absolute risk of breastfeeding with bed sharing. So are mothers who formula feed without bed sharing better mothers than those who breastfeed and bed share? If it’s the absolute risk that counts — as implied by breastfeeding researchers — that’s the inevitable conclusion.
How about homebirth? The absolute risk of death from homebirth with an American homebirth midwife was found to be 5.6/1000 (1 in 179) in a 2012 analysis of Oregon state data. That’s more than 100X higher than the risk of death from bed sharing while breastfeeding. If it’s the absolute risk of death that counts, those women are monsters.
The NPR piece suggests:
…[A]ll bed-sharing is not the same. It doesn’t add the same amount of risk for all families. And so perhaps recommendations about it shouldn’t be the same? Maybe they should be tailored for each family and their circumstances?
How ironic! Those who insist that bed sharing recommendations should be tailored to individual families are often the same people who think that infant feeding recommendations should NOT be tailored for each family and their circumstances; they believe that every family should received the same recommendation that breastfeeding is best for every baby even though that’s obviously untrue.
But let’s get back to the original question: when is it okay to risk a baby’s death? Is the relative risk irrelevant? Is it only the absolute risk that counts? Who gets to decide?
Please share your thoughts in the comment section.

