Dutch midwife Ank de Jonge is at it again, slicing and dicing data in yet another unsuccessful attempt to show that homebirth is safe.
She thought that she had succeeded in Perinatal mortality and morbidity in a nationwide cohort of 529 688 low-risk planned home and hospital births (2009) which appeared to show that homebirth with a midwife in the Netherlands is as safe as hospital birth with a midwife. Unfortunately for her, the subsequent study, Perinatal mortality and severe morbidity in low and high risk term pregnancies in the Netherlands: prospective cohort study, was a stunning indictment of Dutch midwives, demonstrating that Dutch midwives caring for low risk women (home and hospital) had a higher mortality rate than Dutch obstetricians.
Two months ago, de Jonge in a paper in the journal Midwifery Perinatal mortality rate in the Netherlands compared to other European countries: A secondary analysis of Euro-PERISTAT data that attempted to absolve Dutch midwives, but actually CONFIRMED their poor mortality statistics .
de Jonge continues to slice and dice the Dutch homebirth data is an effort to somehow prove that homebirth is safe, when the data suggests that it is not. Her latest effort is Severe adverse maternal outcomes among low risk women with planned home versus hospital births in the Netherlands: nationwide cohort study. She and her colleagues found:
Overall, 92 333 (62.9%) women had a planned home birth and 54 419 (37.1%) a planned hospital birth. The rate of severe acute maternal morbidity among planned primary care births was 2.0 per 1000 births. For nulliparous women the rate for planned home versus planned hospital birth was 2.3 versus 3.1 per 1000 births (adjusted odds ratio 0.77, 95% confidence interval 0.56 to 1.06), relative risk reduction 25.7% (95% confidence interval −0.1% to 53.5%), the rate of postpartum haemorrhage was 43.1 versus 43.3 (0.92, 0.85 to 1.00 and 0.5%, −6.8% to 7.9%), and the rate of manual removal of placenta was 29.0 versus 29.8 (0.91, 0.83 to 1.00 and 2.8%, −6.1% to 11.8%). For parous women the rate of severe acute maternal morbidity for planned home versus planned hospital birth was 1.0 versus 2.3 per 1000 births (0.43, 0.29 to 0.63 and 58.3%, 33.2% to 87.5%), the rate of postpartum haemorrhage was 19.6 versus 37.6 (0.50, 0.46 to 0.55 and 47.9%, 41.2% to 54.7%), and the rate of manual removal of placenta was 8.5 versus 19.6 (0.41, 0.36 to 0.47 and 56.9%, 47.9% to 66.3%).
Conclusions: Low risk women in primary care at the onset of labour with planned home birth had lower rates of severe acute maternal morbidity, postpartum haemorrhage, and manual removal of placenta than those with planned hospital birth. For parous women these differences were statistically significant. Absolute risks were small in both groups. There was no evidence that planned home birth among low risk women leads to an increased risk of severe adverse maternal outcomes in a maternity care system with well trained midwives and a good referral and transportation system.
There’s just one teensy, weensy problem. de Jonge left out the mortality rates. Severe maternal morbidity is an appropriate measure of safely ONLY when death rate is zero or nearly zero. If the death rate is not zero, that MUST be taken into account in assessing safety.
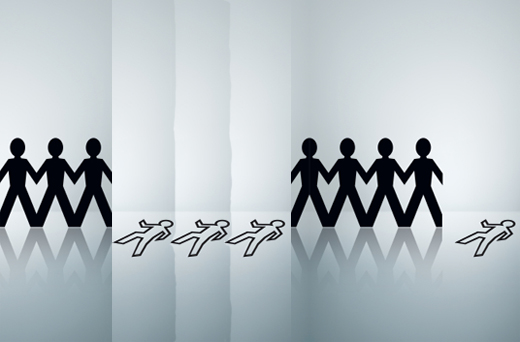
To understand the problem, it helps to look at a graphical representation. The image below compares the incidence of severe maternal morbidity in two groups.
It’s easy to see that there were a greater number of serious complications in the second group than in the first. It is tempting to conclude that the place of birth for the first group is safer than the place of birth for the second group.
Look what happens, though, when we add the number of women who died in each group.
Now it’s easy to see that the place of birth of the first group is far more dangerous than that of the second group. Notice that the rate of serious SURVIVABLE maternal complications is unchanged. But the dead women had complications, too, and they can’t be excluded simply because they died. If 6 women have serious complications in the first group and 3 die, compared to 5 women in the second group who suffer serious complications, and one dies, we CANNOT conclude that the group that had more survivors is the safer group.
de Jonge has shown us the equivalent of the first image, but it’s meaningless unless she shows us the equivalent of the second image. In other words, the MOST important piece of information, the information we MUST have in order to draw conclusions about safety is missing from the new paper and its absence is both inexplicable and impossible to justify. de Jonge does not explain what she did with the maternal deaths. It appears that she excluded them altogether.
If so, de Jonge compared the number of women who SURVIVED severe complications at homebirth to the number of women who SURVIVED severe complications at hospital birth. She didn’t compare the number of women who EXPERIENCED severe complications in each place. And she didn’t compare how many women DIED at each place. Without that information, de Jonge is not entitled to conclude anything.
This paper doesn’t show that homebirth is safe. In the absence of mortality data, this paper is meaningless.