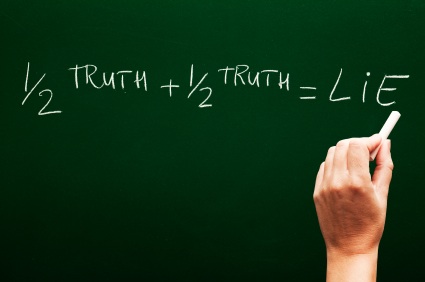
I’ve written many times before about the endless efforts of midwives to demonize interventions in childbirth.
Australian midwife Hannah Dahlen seems to be leading the charge and doesn’t shirk from using deceitful statistics and crappy research to do it.
Dahlen can’t seem to make up her mind about the actual “harms” from interventions. On any given day she might be suggesting that C-section might destroy the infant microbiome, or maybe C-sections might change the epigenetics of neonatal DNA. Today, birth interventions might increase the risk of suicide.
Her central contention is this:
So death from suicide and trauma rises significantly between nine and 12 months after birth; it is nearly four times the rate compared to the first three months following birth.
And:
The women who died had higher rates of intervention in birth, higher rates of early-term births, pregnancy complications and neonatal intensive care admissions. They also tended to have babies who were born with a low birth weight and were ten times more likely than other women to have their baby die.
Her “research” was published in a journal I’ve never heard of, with an impact factor of 2.8. To put that in perspective, high quality journals have impact factors ranging from 30-50.
It’s hardly surprisingly that Dahlen had to resort to publishing in one of the lowest ranked journal in the world. The “research” is crap.
Here is the central claim:
So death from suicide and trauma rises significantly between nine and 12 months after birth; it is nearly four times the rate compared to the first three months following birth.
Sounds impressive until you give it a modicum of thought.
1. Why are suicide and trauma lumped together? There’s a big difference (in cause, effect, a preventive approaches) between dying at your own hand and dying in a car accident. There is no possible justification for including trauma in an analysis like this besides artificially inflating the purported scope of the problem.
2. How does the supposed high suicide rate in the postpartum year compare to the suicide rate for women in the same age group who did not give birth in the past year? Dahlen doesn’t bother to tell us. So we have no idea whether the rate of suicide and trauma is any different following childbirth than it is in women who haven’t given birth. That’s a stunning oversight.
3. Dahlen notes that the suicide rate in the 4th quarter of the postpartum year is more than 3 times higher than the 1st quarter of the postpartum year and implies that this is a dramatic rise. However, it is equally likely that the suicide rate in 3 months after birth drops and then rises again to baseline over the rest of the year. Without the background rate of suicide in women of childbearing years, it is impossible to determine what has actually happened.
4. Dahlen acknowledges that the woman who died of suicide and trauma differed substantially from the rest of the population.
A large proportion of women who died from suicide (73%) had a history of mental illness or substance abuse, or both. Most of the women who died because of accidental injury also had a history of mental illness or substance abuse (or both).
How does that compare to non-postpartum women who commit suicide? Dahlen does’t bother to check. What is the suicide and trauma profile of the other 27% of women? Does it mimic that of women with previous mental illness or substance abuse? Dahlen doesn’t bother to check.
5. Dahlen acknowledges that the neonatal death rates among the women who subsequently died of suicide or trauma were 10 times higher than the death rate of women who did not die of suicide or trauma. Yet she did not ask the glaringly obvious follow up question. Was the purported increase in maternal death from suicide or trauma the result of grief and loss, and not the result of being postpartum.
The bottom line is that Dahlen could not get this paper published in anything other than an extremely low ranking journal because the paper doesn’t show anything. Dahlen waves a bunch of statistics around but fails to investigate whether those isolated statistics mean anything at all, let alone anything about suicide in the postpartum year.
Dahlen’s solution is to provide more “services” to women in the postpartum year. Yet Dahlen utterly failed to show (she didn’t even bother attempt to show) that being postpartum is the relevant risk factor, let alone that more services would decrease the rate of bad outcomes.
If this is what passes for quantitative “research” in Australian midwifery, the solution may not be more services for patients, but better basic math and logic education for midwives.