Ideas have consequences.
Bad ideas about childbirth have deadly consequences.
If you want to understand what went wrong with UK midwifery, read what midwives have written and said:
1. Royal College of Midwives (2006):
“Louise Silverton, the RCM’s deputy general secretary, said it was the responsibility of midwives to encourage women to have a more natural birth.
“Epidurals provide effective pain relief but, where there is no clinical indication that they are necessary, they can significantly raise the likelihood of other interventions such as instrumental deliveries or Caesarean sections occurring,” she said.
“The United Kingdom already has an extremely high Caesarean rate and, as the acknowledged experts in normal pregnancy, labour and birth, we midwives need to debate ways in which we might help to bring this rate down.””
2. Royal College of Midwives 2007/2008:
“Care based on robust evidence probably has the highest profile it has ever had within midwifery. However, if policies, protocols, guidelines and pathways of care are too rigid and are unable to be applied flexibly, then there is a risk that midwives are unable to feel empowered to practice the art of midwifery. They need to use the intuition that experience and knowledge brings, to sense when a problem may or may not be occurring.”
3. Including the nonrational is sensible midwifery (2008)
“ We expose the limitations of pure rationality in the context of childbirth and use the concept of safety to exemplify the limitations that pure rationality imposes. The paper draws on philosophical and spiritual theory to present an analysis of ideas about mind, body, soul and spirit… This revised conceptualisation provides a theoretical basis that allows for and promotes more possibilities and thus more holistic ways of knowing in midwifery.”
4. Including the nonrational is sensible midwifery (2008):
“For example, when a woman and midwife have agreed to use expectant management of third stage, but bleeding begins unexpectedly, the expert midwife will respond with either or both rational and nonrational ways of thinking. Depending upon all the particularities of the situation the midwife may focus on supporting love between the woman and her baby; she may call the woman back to her body; and/or she may change to active management of third stage.”
5. Normal Childbirth: Evidence and Debate by Soo Downe (2008):
“The implication of the new subatomic physics was that certainty was replaced by probability, or the notion of tendencies rather than absolutes: ‘we can never predict an atomic event with certainty; we can only predict the likelihood of its happening’… This directly contradicts the mechanistic model we explored above, and it implies that a subject such as normal birth needs to be looked at as a whole rather than its parts…”
6. Promoting Normal Birth – Research, Reflections and Guidelines (2011)
“ You may have wondered, on first seeing this book, why the title includes the word ‘promoting.’ Why should normal birth be promoted particularly? The answer is simple. Other forms of birth — those involving plenty of interventions, especially cesareans — get plenty of promotion, simply because they may appear to be the easiest option for caregivers or the least frightening ones for pregnant women…”
7. Critical realism: an important theoretical perspective for midwifery research (2014)
“The methods utilised in these studies [of dystocia] have been randomised controlled trials … [which] promises certainty in addressing the condition, based as they are on a positivist epistemology (knowledge that is always true and generalisable) … However, the incidence of dystocia and its negative consequences for women continues to rise. If researchers had grasped the limitations of their research methods by critiquing their ontological and epistemological underpinning, they might have asked different questions about the aetiology of dystocia, researched different interventions to manage it and ultimately had a greater impact on women’s outcomes and experience.”
8. Royal College of Midwives (2015):
“This is part of the intent of the RCM Better Births Initiative, which has three themes, including: The promotion of normal births for majority of the women and normalisation for all women”
9. Cathy Warwick, Royal College of Midwives (2017):
“If women and babies are to be kept safe it is important that their birth, whether straightforward or complex, is kept as normal – or physiological or straightforward or optimal – as possible.”
10. Advocating for evidence in birth: Proving cause, effecting outcomes, and the case for ‘curers’ (2019):
“…[W]hat if evidentiary practice were expanded to include the non-rational? Stengers also has a category into which midwives who do not seek belonging via rationality might fall, a third category of ‘curers’ who ‘are not haunted by the idea of being able to disqualify others, but rather who have cultivated an “influencing practice”’ Such curers are not concerned with being rational … much less with proving (as a doctor-scientist is)…”
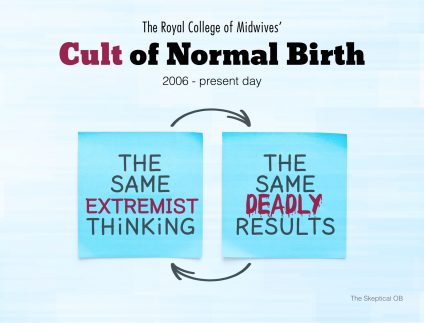
Over and over again the UK midwives trumpet the same extremist thinking and than are shocked to find that babies and mothers suffer the same deadly results.
It’s time to end — once and for all — midwifery allegiance to the cult of normal birth.

