Ahhh, the power of the press release.
How else to explain the fanfare with with the latest Cochrane Review on delayed cord clamping was greeted despite the fact that it showed almost no benefit?
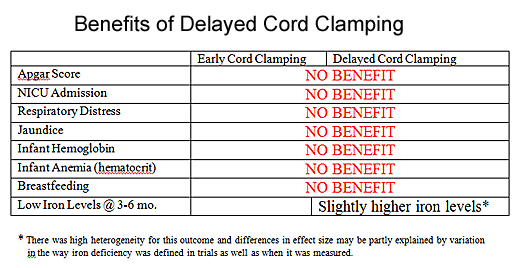
To see what I mean, I’ve created the following chart listing all the benefits of delayed cord clamping.
As you can see, the authors looked at a variety of possible benefits of delayed cord clamping and found almost nothing … except slightly higher iron stores (a laboratory value), one that has no clinical effect and probably has no clinical significance.
So why did mainstream media outlets like the New York Times wax rhapsodic on the front page?
But a new analysis has found that delaying clamping for at least a minute after birth, which allows more time for blood to move from the placenta, significantly improves iron stores and hemoglobin levels in newborns …
Um, not exactly. Obviously babies subject to delayed cord clamping had higher hemoglobin levels in the first few days after birth; they got more blood. But that doesn’t mean that higher hemoglobin levels are beneficial and, indeed, the higher hemoglobin levels did not translate to better Apgar scores, less respiratory distress, fewer NICU admissions, or greater breastfeeding success.
Moreover, it did not translate to lower levels of anemia at 3-6 months. Babies in both groups had the same hemoglobin level and hematocrit at that point, suggesting that the initial transfusion of blood from the cord was unnecessary and the baby had to destroy those blood cells to get to a normal hematocrit.
Not surprisingly, babies who had to destroy blood cells ended up with higher iron stores, but there is no evidence that they benefited from this in any way. Indeed, it would be helpful to look at longer term outcomes to determine if the higher iron eventually disappeared, suggesting no advantage to having higher measures of iron stores. The authors actually acknowledge that the apparent difference in iron stores may not be real, and may reflect disparities in the way that iron stores were measure in the individual studies that make up the meta-analysis.
To understand exactly why there are no real benefits to delayed cord clamping, lets do a thought experiment. Let’s pretend that we gave half of newborns a blood transfusion in the immediate aftermath of birth to test the hypothesis that an immediate blood transfusion benefits normal babies. If we measure the same things that the Cochrane investigators measured, we would get exactly the same results. The only “benefit” would be slightly higher iron levels, and even that isn’t guaranteed since the authors are not sure that result is real.
Would we conclude that routine newborn transfusions offered enough benefits to recommend them? Of course we wouldn’t, since it offers no clinical benefits at all.
The exact same thing can be said about delayed cord clamping.
So what’s this paper really about? This paper is about midwives and natural childbirth advocates dissing obstetricians. Indeed the paper was written by midwives who are desperate to find yet another reason to criticize obstetricians. Delayed cord clamping is just a reaction to the fact that obstetricians have traditionally clamped the cord early. As the chart clearly shows (no chart was included in the study since it would have graphically displayed the lack of benefit), there is no clinical benefit to delayed cord clamping and only a difference in laboratory values at 3-6 months that has no bearing on health and may not be really anyway.
Fortunately, delayed cord clamping appears to have no harms, so there’s no reason that we can see (at the moment) not to do it if parents request it. By that reasoning, we could give every newborn a blood transfusion if their parents request it.
So why is everyone jumping up and down about this study?
That’s the power of the press release … and a paper written to maximize clinically irrelevant effects and minimize the absence of clinical benefit.