A new study recently published in the Journal of Human Lactation, is making the rounds in lactivist circles. However, the study, in addition to being underpowered to reach any conclusions, treats lactating women as if they are nothing more than cows, reducing them to the characteristics of the milk they produce, without any regard to their pain, needs and desires.
The study is Relationship between Use of Labor Pain Medications and Delayed Onset of Lactation by Li et al. and the findings are:
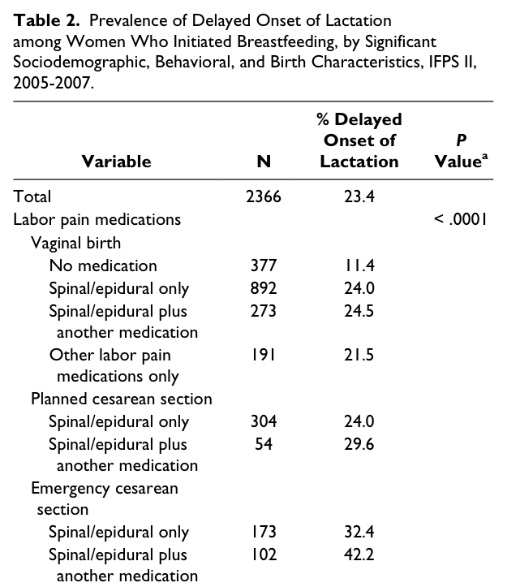
Overall, 23.4% of women in our sample experienced DOL. Compared with women who delivered vaginally and received no labor pain medication, women who received labor pain medications had a higher odds of experiencing DOL: vaginal with spinal/epidural only (aOR 2.05; 95% CI, 1.43-2.95), vaginal with spinal/epidural plus another medication (aOR 1.79; 95% CI, 1.16-2.76), vaginal with other labor pain medications only ([not spinal/epidural]; aOR 1.84; 95% CI, 1.14-2.98), planned cesarean section with spinal/epidural only (aOR 2.13; 95% CI, 1.39-3.27), planned cesarean with spinal/epidural plus another medication (aOR 2.67; 95% CI, 1.35-5.29), emergency cesarean with spinal/epidural only (aOR 2.17; 95% CI, 1.34- 3.51), and emergency cesarean with spinal/epidural plus another medication (aOR 3.03; 95% CI, 1.77-5.18).
The authors concluded:
… [M]others who received pain medications during labor and delivery were more likely to report that they experienced DOL. Because 83% of mothers in the U.S. use pain medication during labor and delivery, the implications of a link found between labor pain medications and onset of lactation, if causal, is of public health and clinical impor- tance.
How did the authors assess delayed onset of lactation? They used a notoriously unreliable method, a questionnaire, which asked mothers to recall the answer to a remarkably vague question:
“How long did it take for your milk to come in?” (1 day or less, 2 days, 3 days, 4 days, more than 4 days).
That’s only one of the six serious limitations to the study acknowledged by the authors:
This study is subject to at least 6 limitations. First … the study sample is not representative of the US population … which prevents generalization of our findings to the entire US population. Second, IFPS II [the questionnaire] did not collect information regarding dose of labor pain medication used ..; therefore a dose-response relationship between pain medication dosage and risk for DOL could not be examined. Third, while overall this was a large study, there were relatively small percentages of mothers exposed to some of the pain medications, which … limited our ability to evaluate the effects of specific medications. Fourth, because we are unable to separate cesareans from labor pain medication use, we are unable to evaluate the effects of the medications used independent of method of delivery. Similarly, we are unable to separate the pain associated with labor/delivery from the use of labor pain medications; therefore, we are unable to tease out whether it is the pain or the pain medications leading to the associations that we observed with DOL. Fifth, data regarding labor course were not collected in IFPS II; therefore we were unable to adjust for labor characteristics such as length of labor, length of second stage labor, or labor/delivery stress, all of which are known to be associated with DOL. Finally, all data were self-reported; hence outcome and exposure misclassification are potential limitations of the study.
So the design of the study itself renders the conclusions virtually useless, and that’s even before we get to the fact that the study is so underpowered that the conclusions are statistically useless.
The number of women in the study as a whole was small, and the number of women in each subgroup was tiny, rendering any conclusions highly suspect from a statistical point of view.
The bottom line, therefore, is that the conclusions of the study are meaningless.
Let’s leave aside for the moment the fact that the authors failed to adequately support their conclusions, and failed to demonstrate that the parameter they are measuring was even remotely clinically relevant (since they never looked at the health of the babies). The study does shed some light on another important issue: the tendency of lactivists to treat women like cows, obsessing about the quality and quantity of their milk, with no regard to the well being of the women themselves. I cannot think of any other study in the literature that rests on the presumption that treating excruciating pain is optional and possibly undesirable, but that is the foundational assumption of this paper. The implicit message of the authors is that women should forgo pain medication in order to “optimize” their breastmilk.
This is especially ironic in light of the confluence between natural childbirth advocacy and lactivism. Evidently the mother’s “birth experience” and desire to avoid lifesaving interventions and C-sections is supposed to take primacy over the baby’s interest in being born alive and neurologically intact. But the situation is magically reversed when it comes to breastfeeding. The mother’s experience is completely irrelevant and all that matters is optimizing the breastmilk that the baby receives.
How, in good conscience, can any group of investigators completely dismiss the mother’s pain in labor? How can they, in good conscience, presume to sway women against pain relief in labor in favor of a highly theoretical benefit that they are incapable of demonstrating even exists? It’s apparently very easy. In the world of lactivism, the wellbeing of the milk producer is irrelevant; only the consumer matters. Here’s what I’d like to know: how is that different from treating women like cows?