It looks like I’m not the only one shocked by the response of UK midwives to the Morecambe Bay Report that places the blame for the preventable deaths of 11 babies and 1 mother squarely on midwives and their pursuit of “normal birth.”
According to the author of the report, Dr. Bill Kirkup:
All showed evidence of the same problems of poor clinical competence, insufficient recognition of risk, inappropriate pursuit of normal childbirth and failures of team-working.
In fact:
The midwives at Furness general were so cavalier they became known as “the musketeers”.
In an interview with reporter Shaun Lintern in yesterday’s Health Service Journal, Dr. Kirkup expressed his disappointment with the response (or, more accurately, the lack of response) from professional bodies. He singled out midwives in particular:
…[He] had also been “concerned” by some comments online which he described as “defensive.”
This included blogs by midwives suggesting the report was anti-midwives or against normal birth, while on social media relatives of those who suffered poor care at Morecambe Bay had been accused of “midwife bashing” and “retrospective negativity.”
This is a direct reference to last weeks’ Twitter chat held by WeMidwives that I wrote about in Being a UK midwife means you never have to say you’re sorry.
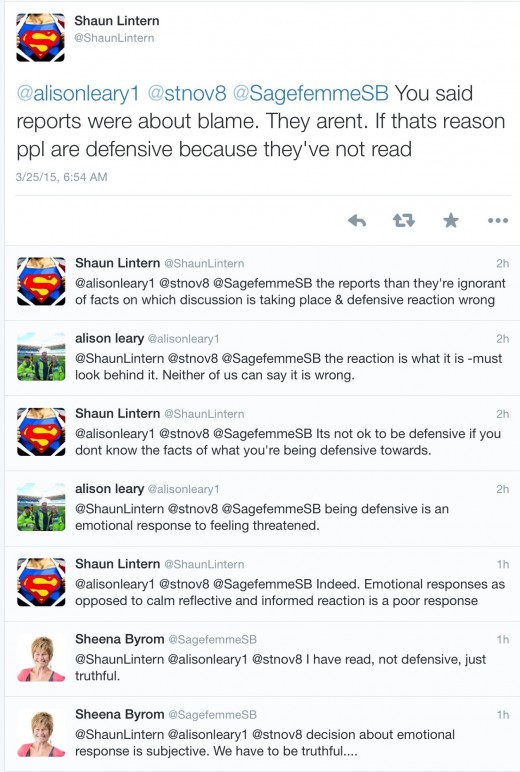
Indeed, midwifery leaders like Cathy Warwick and Sheena Byrom and their colleagues have been holding an impromptu master class on shirking responsibility, such as the Twitter response when Lintern tweeted highlights of the Kirkup interview and Sheena Byrom disparaged them as concerned with “blame.”
But Byrom is hardly alone in her desperate efforts to avoid accountability both for the specific tragedies at Morecambe Bay and for the midwifery philosophy of promoting normal birth that led to these tragedies (and others).
What methods have UK midwives used?
1. Ignoring the report
The report has been greeted in the midwifery community with the sound of silence. Cathy Warwick of the Royal College of Midwives has perfected the art of using a lot of words to say absolutely nothing. In posts on her blog, such as this, she has issued meaningless platitudes and resolutely refused to discuss the core issues in the report.
2. Self-pity
Monday’s piece by an anonymous midwife in The Guardian (I loved being a midwife but bullying, stress and fear made me resign) is a sickening example of how midwives think everything is about themselves and their feelings, patients be damned. See the midwife turn the poor outcome* of a baby at her hands because she failed to recognize the severity of fetal distress into a tale of HER suffering:
The fetal heart is bad – but not bad enough to act. You continue this dance for hours until suddenly the heart trace is terrible – this baby is in real trouble. You press the emergency bell and the world runs into the room. You roll the woman this way and that, attach name bands and tape up earrings, you hold her hand as she is anaesthetised and whisper that the baby will be out soon. You knew something was wrong, but you didn’t have the words and no one listened.
Apparently the fetal heart rate was bad enough to act, but the midwife lacked the clinical competence to recognize it. She “didn’t have the words”??!! What does that even mean? How hard is it tell someone, ” the fetal heart rate indicates this baby is in distress”? Not hard at all, but the midwife didn’t do it.
3. Decrying a culture of “fear”
This is the meme of the moment in midwifery. Midwives are wailing about being held to standards, subject to scrutiny, and forced to use checklists. What fear are they fighting. They’re fighting the fear of preventable maternal and neonatal deaths, the very things that these measures are designed to prevent.
This stunningly immoral and reflects a preoccupation with midwives’ “experience” over patients health and wellbeing.
4. Insisting that it is critical to “avoid blame”
This is the classic maneuver of anyone who fears accountability, but there are some situations in which blame is not merely appropriate, but absolutely necessary for the well being of all.
Imagine a drunk driver who killed a small child in an accident that occurred precisely because he was drunk. What if he told the judge that he should be allowed to go on his merry way because he didn’t intend the child should die, and therefore it is critical to “avoid blame”? We’d be rightly appalled.
The same principle applies to midwives who didn’t mean for babies and mothers to die preventable deaths because they were too committed to “normal birth” to call for interventions. They were to blame. Their philosophy of promoting “normal birth” is deadly and it is appropriate that we blame it and change it.
5. Insisting that problems can only be solved by “positivity” not negativity
That is just stupidity.
6. Banishing the deaths at Morecambe Bay to the “past”
Deaths due to drunk driving, faulty pharmaceuticals, and even intentional murder are all in the past, too. That doesn’t mean would shouldn’t look at them, learn from them, and hold those responsible for them to account.
7. Bullying on social media
Dr. Kirkup specifically noted the bullying that James Titcombe has been subjected to by midwives who think their professional autonomy is more important than whether other people’s babies live or die. He may not even be aware that WeMidwives chose to forward their “concerns” to his employer, the Care Quality Commission. What were they “concerned” about? He quoted me, whom they despise and fear (rightly so, since I intend to hold them to account). It is obviously pointless to bully me, so they tried to bully him.
and, most importantly,
8. Refusing to apologize
How hard is it to say, “We’re sorry. We allowed our preference for ‘normal birth’ to interfere with our ethical obligation to protect the health and well being of mothers and babies.”?
Apparently it’s very hard because it would require acknowledging the central moral and empirical defect at the heart of contemporary midwifery culture, the obsession with “normal birth.” Midwives have convinced themselves that normal birth isn’t merely better for them, it’s better for their patients. Acknowledging the many preventable deaths that followed ineluctably from this deadly philosophy would mean a wholesale attitude readjustment. Instead of viewing themselves as “guardians of normal birth” they’d be relegated to what they are in reality, mid-level maternity providers who are legally and ethical required to call high level providers like obstetricians, pediatricians and anesthesiologists even when it means sacrificing autonomy.
Unfortunately, for midwives, self-justification and preservation of their own autonomy takes precedence.
I consider myself a very cynical person, but even I am shocked by the brazen behavior of UK midwives. Not only do they feel no remorse for the preventable deaths at the hands of their colleagues, they feel free to flaunt their lack of remorse on social media. Not only do they refuse to be held accountable, they feel free to criticize anyone who dares hold them accountable. Not only do they refuse to recognize the full breadth of human suffering that took place at Morecambe Bay, they feel free to compound that suffering by chastising and bullying the sufferers.
To Cathy Warwick, Sheena Byrom and other UK midwifery leaders I say this:
Have you no shame??!!
*Edited 3/25/15 10 PM from “died” to “poor outcome” to reflect the fact that the midwife does not disclose what happened to the baby.