Apparently the author started with the conclusions, spoke only to those who would support that conclusion, and failed to consult even a single expert on the topic to produce a hatchet job on electronic fetal monitoring (EFM).
Noah Berlatsky wrote The Most Common Childbirth Practice in America Is Unnecessary and Dangerous for The New Republic (TNR).
…[W]hy despite decades of overwhelming evidence, do doctors and patient alike continue to insist on this largely useless and sometimes dangerous procedure?
The obvious answer is that the author doesn’t understand the issue. What’s more likely, that obstetricians are engaged in a world-wide plot to harm mothers and babies, or that Noah Berlatsky, a journalist with no medical training, doesn’t understand the state of the evidence?
[pullquote align=”right” color=””]An author writes a piece decrying obstetric technology without ever consulting an obstetrician and editors think that is acceptable?[/pullquote]
You might think, therefore, that the editors at TNR would have considered that Berlatsky didn’t understand what he was talking about, and insisted on consultation with and quotes from experts in the issue, obstetricians. You would be wrong. It was awesome click-bait, one sided and shocking. They published it, and when the deficiencies of the piece were pointed out to Berlatsky, he resorted to name calling, deleting and blocking.
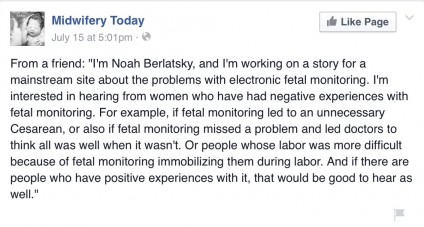
The piece reads as if Berlatsky consulted only the natural childbirth industry who profit by demonizing modern obstetrics. And, indeed, that is precisely what he did. He quoted midwives and an executive from the Childbirth Connection, the largest natural childbirth lobbying organization. Then he reached out to lay midwives searching for EFM bad outcomes with which to frame his piece.
…I’m interested in hearing from women who have had negative experiences with fetal monitoring. For example, if monitoring led to an unnecessary Cesarean, or also if fetal monitoring missed a problem and led doctors to think all was well when it wasn’t…
There is so much wrong with the piece that I can’t recount it all. The single biggest problem with it is that the issue of EFM is complicated, nuanced and poses difficult choices. To understand that issue, you need to understand what EFM is and why it was created.
Childbirth is inherently dangerous. The day of birth is the single most dangerous day of the 18 years of childhood. Every newborn death is a dreadful tragedy, but the cruelest form of newborn death may be stillbirth during childbirth. A woman labors in agony for hours, pushes with all her strength to expel the baby and finally the baby is born … dead. During labor, the baby was deprived of oxygen (fetal distress) and died. If the baby had been delivered by C-section, it almost certainly would have survived.
Before C-sections became very safe, the issue was moot. There was no point in monitoring the baby during labor if you couldn’t do anything to save the baby. The advent of safe C-sections gave impetus to efforts to diagnose fetal distress and deliver babies before they could be harmed or killed.
Unfortunately, unborn babies are inaccessible. You can’t measure their oxygen levels, or their blood pressure, or examine them. The only thing you can measure is their heart rate. Determining health from heart rate is exceedingly difficult and imprecise. You have to listen at the right times and for long enough to detect harmful changes; electronic fetal monitoring was designed to monitor the fetal heart rate for long periods and to create a written record.
Fetal monitoring, first using handheld listening devices and later using EFM, essentially eliminated stillbirth in labor. This success in nearly eliminating stillbirth in labor encouraged obsetricians to believe that they could eliminate cerebral palsy if they monitored more, longer and with more sophisticated techniques. It wasn’t until EFM was in widespread use that we came to understand that while oxygen deprivation causes cerebral palsy, oxygen deprivation is not the only thing that can cause cerebral palsy.
So where are we know?
1. Fetal monitoring, using listening devices or EFM, has been spectacularly successful in preventing stillbirth during labor.
2. EFM has very high sensitivity. If a baby is experiencing oxygen deprivation, EFM will alert providers.
3. We have come to understand the EFM has low specificity. That means that it can signal fetal distress when no distress is present, leading to unnecessary C-sections.
4. EFM provides proven benefits in high risk pregnancies. That’s not surprising since EFM is a screening test and all screening tests are more accurate in high risk populations than in low risk populations.
5. EFM can probably prevent some forms of cerebral palsy, but many probably occur before the onset of labor and EFM can’t prevent those cases.
6. In low risk populations, EFM probably provides no advantage above listening to the fetal heart rate following a strict pattern of frequent listening, which essentially requires one on one nursing in labor and delivery suites. This is a critical point: Even in low risk populations EFM is not useless, it’s just no better than listening to the heart rate according to a strict schedule. And in high risk populations, EFM has been repeately shown to improve outcomes.
7. There is no evidence that EFM is dangerous. To be dangerous, EFM would have to lead to poorer outcomes and it does NOT lead to poorer outcomes. Why then do natural childbirth advocates demonize EFM? The reason is not outcome, but process. Natural childbirth advocates are obsessed with process and take a good outcome for granted. Doctors are more concerned with outcome than process, and eons of human history have shown that a good outcome can never be taken for granted.
8. Oxygen deprivation in labor is still a serious problem requiring our best efforts to prevent it. Is EFM the best possible tool to prevent oxygen deprivation? It’s not the best, but at the moment, it’s one of the few things we have.
Berlatsky and his those he chose to quote are anxious to demonize EFM, but they don’t appear to be the least bit concerned about how to prevent brain damage and infant death. They don’t offer other better methods to protect babies; it appears to never enter their minds that there is anything that can or should be done to protect babies.
And that’s the critical difference between natural childbirth advocates like Berlatsky and the people he quotes and obstetricians. They’re willing to settle for things the way they are now; that’s good enough for them. Obstetricians are NOT willing to settle. They want every baby they deliver to be healthy; they want every mother they deliver to be healthy. They will continue working toward that end.
In the meantime, people like Berlatsky, who doesn’t understand the underlying issues, will continue writing crappy pieces that demonize technology; and continue to pretend that obstetrics ought to be like horse-shoes and hand grenades: close enough is good enough. Berlatsky is entitled to his uninformed opinion; but there was no reason for TNR to publish such a misleading, unbalanced, biased piece.
An author writes a piece decrying obstetric technology without ever consulting an obstetrician and editors think that is acceptable? If so, journalism has reached a sorry state.