
The sky is falling! The sky is falling!
That’s the impression you might get from an article in today’s Guardian, ‘A third of people get major surgery to be born’: why are C-sections routine in the US?
Caesareans have transformed from life-saving intervention into risky procedure performed for one in three births – and often geography is the deciding factor.
Yet the scientific evidence shows that the demonization of C-sections is based on ideology and contradicted by data.
Ideology oozes from nearly every quote in the piece.
“We are quite worried when the C-section rate goes above 30%, as it is in the United States,” said Dr Flavia Bustreo, the assistant director general for family, women’s and children’s health at the World Health Organization…
A C-section rate of 10% to 15% is “natural”, she said. “Above 15%, you don’t have additional benefits, and you have the risks, and you have the unnecessary health costs.”
There is no such thing as a natural C-section rate. Perhaps Dr. Bustreo means that a C-section rate of 10-15% is “optimal,” but that’s not what the scientific evidence shows.
In fact, some experts believe this rise in caesareans is one of the many intertwining factors contributing to crisis rates of maternal mortality, or death, and morbidity – defined as significant injury related to a pregnancy – which are increasing in the US even as they fall in other first-world countries.
“It’s certainly one of the downstream consequences” of performing avoidable C-sections, said Jill Arnold, who runs a website, The Unnecesarean, that tracks individual hospitals’ C-section rates …
Jill Arnold is not an expert. She’s a lay person and an ideologue. And she has no data that shows that C-section increase maternal mortality because there isn’t any.
“A third of people get major surgery to be born,” said Dr Neel Shah, a research physician at Beth Israel Deaconess Medical Center who works on ways to reduce avoidable C-sections.
As someone who had a 16% C-section rate when I practiced, I find myself mystified by a C-section rate of over 30%, but that, in itself, is not a reason to demonize C-sections. A third of the people in the US need glasses for nearsightedness yet we don’t conclude that glasses are over prescribed.
“It is very, very clear to me the connection between the number of C-sections and mortality and morbidity,” said Dr Shah.
I don’t know how it could be clear to him that C-sections increase maternal mortality since his OWN data show precisely the opposite.
Relationship Between Cesarean Delivery Rate and Maternal and Neonatal Mortality was published in JAMA in 2015. The authors, including Dr. Shah, concluded:
The optimal cesarean delivery rate in relation to maternal and neonatal mortality was approximately 19 cesarean deliveries per 100 live births.
They graphed their data:


These graphs show that C-section rate below 19% lead to preventable maternal and neonatal deaths. In other words, they show that the WHO “optimal” rate, far from being optimal, is actually deadly.
They also show that C-section rates above 19% are NOT harmful. There appears to be NO increased risk of either maternal or neonatal mortality for rates as high as 55%.
US maternal mortality statistics show that most of the leading causes of maternal death have nothing to do with C-sections.
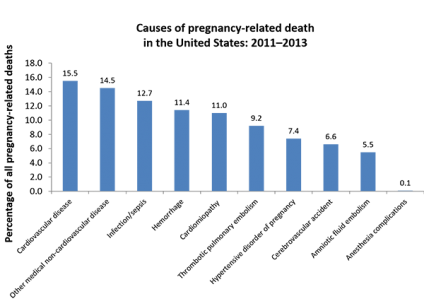
The most important message in this graph is that fully 41% of US maternal deaths are caused by cardiovascular (including cardiomyopathy) and non cardiovascular diseases. And that reflects the fact that pregnant women are now older, more obese and suffering from more chronic diseases than ever before. There’s no evidence that a high C-section rate contributes to maternal mortality.
Indeed, Gene DeClercq, a professor at the BU School of Health echoes my view:
… Declercq, who notes he is “no fan of unnecessary C-sections”, says the bigger drivers of maternal mortality probably include factors like the opioid crisis and the fact that many new mothers are dropped from Medicaid, the government-run health program, shortly after they give birth.
Just addressing the C-section rate alone won’t reduce the maternal mortality rate. Other developed countries have C-section rates that are as high as the United States’. A 2012 international comparison found that the C-section rate was 21.8% in Norway and 24.4% in the UK but 31.7% in Germany and 38.8% in Canada.
Despite the claims of C-section alarmists, the sky is not falling.
But even if it were, wailing and gnashing of teeth, the preferred response of those who demonize C-sections, would not accomplish anything. That’s because the driver of C-section rates is uncertainty. We know that lack of oxygen during labor, either from placental insufficiency, trapped head during a breech birth or severe shoulder dystocia can lead to permanent brain damage and death of babies. Unfortunately, we don’t have an accurate way of determining IN ADVANCE which babies will be injured during birth.
We are forced to resort to crude methods like measuring the baby’s heart rate to determine if it is at risk, and therefore are forced to perform C-sections that turn out to be unnecessary in retrospect. We know that some babies will die during breech birth because their heads will get trapped but we have no way of predicting in advance which babies will get stuck and therefore we recommend routine C-section for breech even though we know that nearly all of those C-sections are unnecessary. We know that some babies, particularly large babies, will suffer serious complications from shoulder dystocia, up to and including death, but we don’t know how to determine which babies will suffer shoulder dystocia so we are forced to recommend C-section in many cases where it is unnecessary.
Natural childbirth advocates like to pretend that the solution to imperfect technology is no technology. Since electronic fetal heart rate monitoring has a high false positive rate, we should just stop using it. Since most breech babies will fit, we should just stop doing C-sections for breech. Since most big babies won’t be harmed by shoulder dystocia, we should simply stop worrying about it.
But the solution to imperfect technology is not forgoing technology; it is improving technology. We need to spend tens of millions of dollars (or more) perfecting a way to determine fetal oxygen levels during labor. We need to spend tens of millions of dollars (or more) perfecting a way to determine whether a specific baby in a specific position will fit through a specific pelvis. When we create such technologies, the C-section rate will drop precipitously because we learn in advance which C-sections are unnecessary and stop doing them.
Wailing about the C-section rate accomplishes absolutely nothing. Crying “the sky is falling” does not prevent the sky from falling; it’s even more irresponsible when the sky is not falling at all.

