
A new paper published yesterday in PLOS compares the long term risks of vaginal birth and C-section.
The paper is Long-term risks and benefits associated with cesarean delivery for mother, baby, and subsequent pregnancies: Systematic review and meta-analysis. In addition to the comparison, it offers an object lesson in the way that researchers frame results in order to lead to a preferred conclusion.
The risk of urinary incontinence from vaginal birth is 10,000% higher than the risk of subsequent accreta.
The authors start with the assumption that C-sections are “bad”:
Rates of cesarean delivery continue to rise worldwide, with recent (2016) reported rates of 24.5% in Western Europe, 32% in North America, and 41% in South America. In the presence of maternal or fetal complications, cesarean delivery can effectively reduce maternal and perinatal mortality and morbidity; however, an increasing proportion of babies are delivered by cesarean when there is no medical or obstetric indication. The short-term adverse associations of cesarean delivery for the mother, such as infection, haemorrhage, visceral injury, and venous thromboembolism, have been minimized to the point that cesarean delivery is considered as safe as vaginal delivery in high-income countries … This notwithstanding, the long-term risks and benefits of cesarean delivery for mother, baby, and subsequent pregnancies are less frequently discussed with women …
The “worst” C-sections are those done without medical indication simply because the mother requested it:
Maternal preferences are an important influence on decisions about mode of delivery. At present, evidence of longer-term complications of cesarean delivery has not been adequately synthesized to allow fully informed decisions about mode of delivery to be made…
Women typically choose maternal request C-sections in an effort to avoid perineal damage leading to pelvic organ prolapse and urinary incontinence. These poor, benighted women apparently aren’t fully informed, though there is no indication that they are any more or less informed than women who choose vaginal birth. No matter!
Here’s how the authors framed their results:
When compared with vaginal delivery, cesarean delivery is associated with a reduced rate of urinary incontinence and pelvic organ prolapse, but this should be weighed against the association with increased risks for fertility, future pregnancy, and long-term childhood outcomes.
The authors imply that the risks for future pregnancy outcomes are comparable to the decrease in urinary incontinence and pelvic organ prolapse. They’re not.
Let’s look at the four most important long risks of vaginal birth and C-sections: pelvic organ prolapse and urinary incontinence vs. subsequent placenta previa or accreta (the most dread complication of all).
One RCT and 79 cohort studies (all from high income countries) were included, involving 29,928,274 participants. Compared to vaginal delivery, cesarean delivery was associated with decreased risk of urinary incontinence, odds ratio (OR) 0.56 (95% CI 0.47 to 0.66; n = 58,900; 8 studies) and pelvic organ prolapse (OR 0.29, 0.17 to 0.51; n = 39,208; 2 studies)… Pregnancy following cesarean delivery was associated with increased risk of placenta previa (OR 1.74, 1.62 to 1.87; n = 7,101,692; 10 studies), placenta accreta (OR 2.95, 1.32 to 6.60; n = 705,108; 3 studies) …
In other words, C-section halves the risk of urinary incontinence, and cuts the risk of pelvic organ prolapse by 70%. However, C-section almost doubles the risk of placenta previa in a subsequent pregnancy and increases the risk of accreta by nearly 200%. Those results seem very impressive until you look at the absolute risk.
Using the numbers provided in the paper, I created these icon arrays to demonstrate the absolute risk of various bad outcomes.
Here are the long term risks of vaginal birth:

Here are the long term risks of C-section:
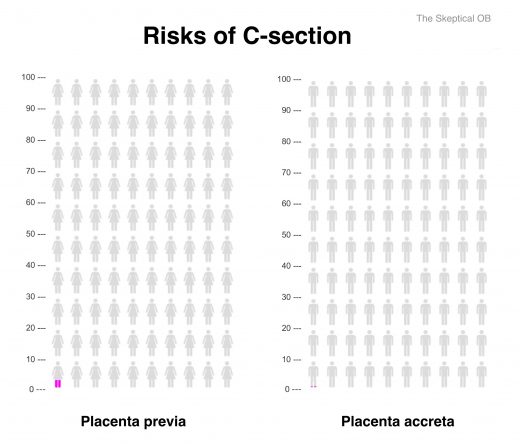
Displaying the data as icon arrays makes it clear that the long term risks of vaginal birth and C-section are not remotely comparable.
The risk of pelvic organ prolapse from vaginal birth dwarfs the risk of accreta from C-section. Indeed, the risk of urinary incontinence from vaginal birth is 10,000% higher than the risk of subsequent accreta. Yes, you read that right, fully 10,000% higher. And the risk of pelvic organ prolapse, while not as great, is still 1000% higher after vaginal birth.
Should we be concerned about placenta accreta as a long term risk of C-section? Of course we should, but we should also put it into perspective. Accreta is a potentially life threatening outcome and every woman should be informed about the possibility before she consents to a C-section. However, the risk is minuscule compared to the life altering risks of pelvic organ prolapse and urinary incontinence.
The authors note:
Although we cannot conclude that cesarean delivery causes certain outcomes, patients and clinicians should be aware that cesarean delivery is associated with long-term risks … for subsequent pregnancies and a reduced risk of urinary incontinence and pelvic organ prolapse for the mother. The significance that women attribute to these individual risks is likely to vary, but it is imperative that clinicians take care to ensure that women are made aware of any risk that they are likely to attach significance to. Women and clinicians thus should be aware of both the short- and long-term risks and benefits of cesarean delivery and discuss these when deciding on mode of delivery.
It would have been more accurate to conclude thus:
Although we must be mindful of potentially catastrophic long term complications from C-section, the risk is dwarfed by the risk of life alterning long term complications from vaginal birth. Since the risk of urinary incontinence from vaginal birth is 10,000% higher than the risk of subsequent accreta from C-section, the choice of maternal request C-section is eminently sensible.
Edited to correct the juxtaposition of the absolute values for urinary incontinence and pelvic organ prolapse.

