NPR recently published a chilling piece.
She Wanted To Be The Perfect Mom, Then Landed In A Psychiatric Unit details the horrifying experience of a woman who suffered from postpartum psychosis.
Lisa wanted to be the perfect mom. She was ready to be the perfect mom. She and her husband lived in San Francisco, and Lisa had worked as a successful entrepreneur and as a marketing executive for a Silicon Valley tech company. When it came to starting her family, she was organized and ready to go. And that first week after her baby was born, everything was going according to plan. The world was nothing but love.
Then the baby started losing weight, and the pediatrician told Lisa to feed her every two hours.
Lisa started to feel like she couldn’t keep up.
“It weighed on me as, ‘I’ve failed as a mom. I can’t feed my child,’ ” she says. “I needed to feed her — that was the most important thing. And my well-being didn’t matter.”
She was barely sleeping. Even when she could get a release from what felt like breastfeeding purgatory, she couldn’t relax. As she got more and more exhausted, she started to get confused.
When she mentioned suicide her husband hospitalized her.
[pullquote align=”right” cite=”” link=”” color=”” class=”” size=””]Where does a woman get the idea she must be a perfect mother? From the same place that some women get the idea that they must be a perfect wife and deserve to be beaten if they are not: she is socialized to it.[/pullquote]
Lisa doesn’t remember any doctors or nurses telling her why she was there or what was going on. But she does remember, about a week into her hospitalization, her husband bringing a printout from online about postpartum psychosis.
The article said elevated hormones from childbirth — plus sleep deprivation — can trigger confusion and paranoia. Lisa didn’t believe it — she thought her husband was tricking her and had spent hours using Photoshop to piece together a fake article.
Suicide claims many women in the year after a baby’s birth:
In the U.S., mental health problems are one of main contributors to maternal mortality, according to a 2018 report from a Centers for Disease Control and Prevention initiative called Building U.S. Capacity to Review and Prevent Maternal Deaths. On the report’s list of causes of death among new moms, mental health problems (which include drug overdoses) rank seventh — nearly tied with the complications of high blood pressure. For white women, mental health problems are the fourth leading cause of death.
Where did Lisa get the idea that her baby needed perfection?
It certainly wasn’t from the baby. As attachment theorist D.W. Winnicott first articulated, a baby needs only a ‘good enough’ mother by which he meant “the ordinary good mother … the devoted mother.”
As a Wikipedia article notes:
…[T]he idea of the good enough [mother] was designed on the one hand to defend the ordinary mother … against what Winnicott saw as the growing threat of intrusion into the family from professional expertise; and on the other to offset the dangers of idealisation …
But we didn’t need an attachment theorist to explain this reality. We are well aware that children can and do bond desperately to parents who abuse them.
I doubt it was from her own experience. Most people love their own mothers dearly despite recognizing (and complaining about) the fact that she is not perfect.
So where did she get the idea that she needed to be a perfect mother? From the same place that some women get the idea that they need to be a perfect wife and merit punishment from their husbands if they are not: she was socialized to it.
For most of human history women have been socialized to the idea that they must be perfect wives; meek, subservient, devoted to meeting any and every need a husband could dream up, no matter how ugly or unreasonable. Women were taught that when they “failed,” they deserved to be punished. Until very recently nearly every culture considered a wife’s body the property of her husband and he had the legal right to beat her, rape her or lock her away forever. Many cultures still do.
Even within our own culture, where we deem wife beating a crime, many women are abused and believe they deserve to be abused if they fail to meet their husbands’ expectations. “It was my fault!” is often the first thing a battered woman will say to the medical provider who discovers her injuries.
Why do women stay with abusive partners? There are a host of reasons but nearly always one of them is that the woman believes she owes her partner perfection and he is entitled to discipline her if she falls short.
Our culture, touting “attachment mothering,” socializes women to believe they owe their babies perfection. And mothers do believe it, eagerly disciplining other women — family, friends, acquaintances on social media — if they “fall short.”
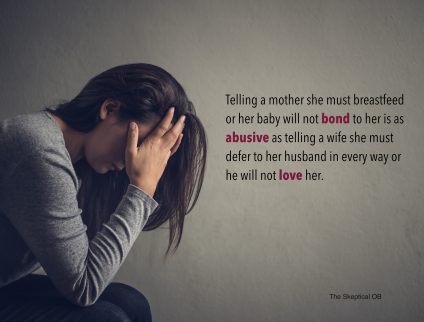
Mothers (and “experts”) verbally abuse women who don’t or won’t comply. Telling a mother she must breastfeed or her baby will not bond to her is as abusive as telling a wife she must defer to her husband in every way or he will not love her. Both are ugly lies that serve no other purpose than to force women’s acquiescence.
Sadly, the journalists at NPR are every bit as socialized to such misogynistic beliefs.
Although they correctly identify the pressure to breastfeed as a trigger for postpartum psychosis, their “solution” is bizarre in the extreme.
The writer of the NPR piece approvingly describes a psychiatric facility designed for postpartum treatment:
Every room has a hospital-grade breast pump, Kimmel says, and there’s a lactation consultant who helps women with breastfeeding. The unit has a designated refrigerator for moms to store pumped milk.
What message does that send? It’s the equivalent of treating a woman who was beaten for burning her husband’s dinner by providing her with a kitchen and a cooking instructor.
It reinforces the same misguided, misogynist beliefs that brought her to this deadly impasse in the first place.
Fortunately, Lisa understood the opposite.
She had a second child but did not suffer a recurrence:
The psychosis did not come back after Vivian’s birth, in part because of all the precautions Lisa took. She made sure she got enough sleep. She gave herself permission to give up breastfeeding if it became too much.
“We’ve got so many messages of just self-sacrifice,” Lisa says. ” ‘Do anything for your kids.’ ‘Drop everything. That’s what it means to be a good mom.’ And for me, that’s not what made me a good mom. That’s what made me fall apart.
Words that other mothers struggling to meet unreasonable goals ought to take to heart. Because babies don’t require perfection from mothers; only other adults do.

