
Breastfeeding research is a flawed paradigm in which statistically illiterate methods, meaningless “benefits” and ideological censorship dominate the literature.
It’s the inevitable result of the fact that lactation professionals made extravagant claims about the benefits of breastfeeding more than a decade before they bothered to check if those claims were true. By now it’s become obvious even to them that their original predictions about lives and healthcare dollars saved and diseases and conditions prevented have utterly failed to materialize. We are constantly treated to ever more desperate efforts to find ever more arcane “benefits” of breastfeeding.
[pullquote align=”right” cite=”” link=”” color=”” class=”” size=””]Breastfeeding did NOT prevent infant hospitalizations for respiratory or GI infections.[/pullquote]
A new paper, Breastfeeding Status and Duration and Infections, Hospitalizations for Infections, and Antibiotic Use in the First Two Years of Life in the ELFE Cohort, is a perfect example.
Spoiler alert: the authors found that breastfeeding didn’t have the anti-infective benefits claimed for it. But that’s not how they presented their findings. Because of ongoing pressure for ideological conformity in breastfeeding research, they concluded:
Predominant breastfeeding for <1 month was associated with higher risk of a single hospital admission while predominant breastfeeding for ≥3 months was associated with a lower risk of long duration (≥4 nights) of hospitalization.
Which is just another way to say breastfeeding does NOT reduce the risk of infant hospitalization.
Let’s see what the authors found and examine how they had to slice and dice the data to arrive at the misleading conclusion.
They start by rehearsing the claims made for breastfeeding benefits:
The World Health Organization (WHO) recommends exclusive breastfeeding for 6 months, or at least the first 4 months of life. These recommendations were mainly based on the protective effect of breastfeeding against infectious morbidity and mortality. In fact, breast milk components, such as immunoglobulin A (IgA) or maternal leukocytes, can both supplement and promote the newborn’s immature immune system and therefore lead to protective effect against infections.
More precisely, recent literature has shown that breastfeeding is related to a reduced rate of hospital admission for diarrhea and respiratory infections as well as a protective effect on otitis media in children up to 2 years old. Of note, otitis media studies were mostly from high-income countries, whereas results on diarrhea and respiratory infection studies were mostly found in settings from low- and middle-income countries. In high-income countries, the preventive effect of breastfeeding on respiratory tract infections is less consistent across studies. In the cluster-randomized trial on promotion of breastfeeding (PROBIT), which took place in Belarus in the 1990s, breastfeeding was related to a reduced risk of gastrointestinal infections in the first year of life.
This is an excellent summary. Contrary to the claims of lactation professionals, the existing research shows that breastfeeding reduces the risk of ear infections in high income countries and respiratory infections and diarrheal illnesses in low income countries.
The authors set out to investigate whether breastfeeding in a high income country (France) reduces the risk of serious respiratory and gastrointestinal infections by looking at the impact of breastfeeding on pediatric hospital admissions.
Here’s what they found:
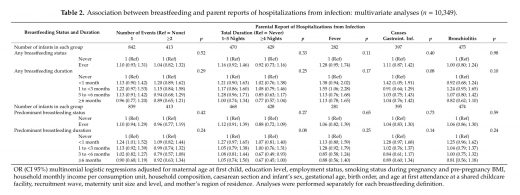
There was NOT EVEN ONE statistically significant association between breastfeeding and hospitalization for fever, gastrointestinal infection or respiratory infection.
Oops!
It’s hardly surprising. No one has ever been able to show that breastfeeding reduces the risk of hospitalization in term infants.
But given the mandated ideological conformity in breastfeeding research, no one was going to publish that inconvenient fact. Therefore, the authors began data dredging, slicing and dicing the data to come up with any association, no matter how arcane.
They looked at parent reported “events” of respiratory infection, ear infection and antibiotic use.
Finally they found a few statistically significant results:

Compared to never-breastfed infants, infants who were predominantly breastfed for <1 month were at higher risk of being hospitalized …
Oops!
How did the authors deal with that finding? They excluded early hospitalizations.
Why? They provide no compelling reason.
Compared to never-breastfed infants, infants who were predominantly breastfed for at least 3 months were at lower risk of long duration (≥4 nights) of hospitalizations…
And:
Compared to never-breastfed infants … any breastfed for <1 month infants were at higher risk of hospitalization from gastrointestinal infections.
Oops!
So they sliced and diced the data even more and finally came up with something:
…[P]redominant breastfeeding for over 3 months was related to lower risk of at least 4 nights of hospitalization up to 2 years, while any breastfeeding for over 3 months was related to higher risk of 1 or 2 bronchiolitis events in the first 2 years of age. Finally, both any and predominant breastfeeding durations were negatively associated with frequency of antibiotic use.
What does this mean? Absolutely nothing because it is an example of data dredging (aka p-hacking).
According to Wikipedia:
Data dredging (also data fishing, data snooping, data butchery, and p-hacking) is the misuse of data analysis to find patterns in data that can be presented as statistically significant when in fact there is no real underlying effect. This is done by performing many statistical tests on the data and only paying attention to those that come back with significant results, instead of stating a single hypothesis about an underlying effect before the analysis and then conducting a single test for it.
Why are these results meaningless?
Conventional tests of statistical significance are based on the probability that a particular result would arise if chance alone were at work, and necessarily accept some risk of mistaken conclusions of a certain type … When enough hypotheses are tested, it is virtually certain that some will be statistically significant but misleading, since almost every data set with any degree of randomness is likely to contain (for example) some spurious correlations…
In other words if a significance level of 0.05 is used (as in this paper), there’s a 5% chance that statistically significant conclusions will be spurious. In a large dataset with only a few statistically significant associations, that virtually ensures that those associations are not valid. Hence data dredging is considered a misuse of data analysis.
The authors of the paper claim:
Even in the context of a high-income country with short breastfeeding duration, we highlighted a lower risk of infectious morbidity related to breastfeeding duration, especially for duration of hospitalization and antibiotic use.
But the truth is they found nothing of the kind.
This is just the latest example of statistically illiterate methods, meaningless “benefits” and ideological censorship that render invalid most of the scientific literature on the benefits of breastfeeding.

