Natural childbirth advocates are obsessed with unmedicated vaginal birth with no interventions of any kind. That’s because they value process over outcome. How a baby is born is apparently more important than whether it is born dead or alive, healthy or brain injured.
Unfortunately, the natural childbirth obsession with process at the expense of outcome has infiltrated conventional medicine. Just as natural childbirth advocates judge hospitals and providers by C-section rates and induction rates, cost cutters and self-appointed avatars of quality like Consumer Reports have fallen prey to woo. Hence the bizarre invocation of C-section rates and induction rates and measures of “quality.”
There’s just one problem. The process of birth has NOTHING to do with the outcome. A new paper in the Journal of the American Medical Association (JAMA) makes that crystal clear. The paper is Association Between Hospital-Level Obstetric Quality Indicators and Maternal and Neonatal Morbidity by Howell et al. A more accurate title would be Oops! There is No Association Between Hospital-Level Obstetric Quality Indicators and Maternal and Neonatal Outcome.
As part of its core measure set, The Joint Commission now recommends 2 perinatal quality measures that address important aspects of obstetric care during childbirth: elective deliveries performed prior to 39 weeks of gestation and cesarean deliveries performed in low-risk nulliparous women. The elective delivery measure, which includes nonmedically indicated deliveries associated with medical induction or cesarean delivery at more than 37 weeks and prior to 39 weeks of gestation, is also mandated by the Centers for Medicare & Medicaid Services.11 The elective delivery before 39 weeks of gestation indicator is intended to reduce neonatal complications among term infants. Assessing rates of cesarean delivery performed in low-risk patients is intended to reduce unnecessary variation in rates of cesarean delivery. Both of these measures may be associated with maternal outcomes. However, how well hospital performance on these quality indicators correlates with maternal or neonatal morbidity is not known.(my emphasis)
In other words, C-section rates and inductions rates became indicators of “quality” without anyone bothering to determine if they had anything to do with quality. Why? I suspect that it is because of the unholy alliance between natural childbirth advocates and cost cutters. Natural childbirth advocates have managed to convince cost cutters that “unhindered” vaginal birth is “better” because it saves money. The truth is that rather different on both counts.
Howell et al. looked at births in New York State in 2010:
… The final sample included 115 742 deliveries, of which 2732 (2.4%) were associated with severe maternal morbidity. Of the 119 793 newborns identified, we excluded 4672 multiple births, 4447 with congenital anomalies, and 7258 with gestational age less than 37 weeks. The final sample included 103 416 newborns; of these, 8057 (7.8%) were associated with neonatal morbidity.
What did they find?
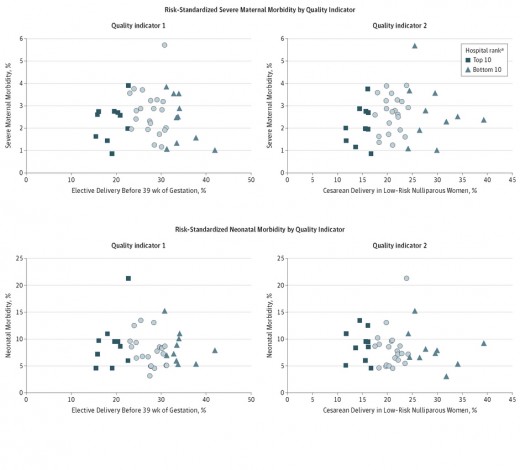
Hospital rankings on both quality measures were not associated with hospital rankings for maternal or neonatal morbidity as demonstrated in the Figure. In fact, among the 10 hospitals with the best performance (lowest rates) on elective deliveries, only 3 were in the lowest quartile of risk-standardized severe maternal morbidity. Among the 10 hospitals with the best performance (lowest rates) on the low-risk cesarean delivery measure, only 3 were in the lowest quartile of risk-standardized severe maternal morbidity. The rankings were similarly discordant for neonatal morbidity.
As the scatter plots show, there is no relationship between C-section rates and outcomes or between induction rates and outcome.
The authors conclude:
… Severe maternal morbidity rates varied 4- to 5-fold between hospitals, and there was a 7-fold variation in neonatal morbidity at term between hospitals. Although there was substantial variation in morbidity rates, they were not correlated with the performance measures designed to assess hospital-level obstetric quality of care.
Our results are consistent with findings from the Maternal Fetal Medicine Network and studies in NICUs demonstrating that performance assessment based on isolated measures do not accurately characterize the overall quality of care in a hospital…
… Our findings highlight the need for an expanded array of obstetric quality measures.
I personally think that the findings highlight the fact that process measures are NOT quality measures.
Contrary to the claims of natural childbirth advocates, C-sections and inductions do NOT lead to an increase in poor outcomes. The key to good outcomes is ensuring the correct match between what a patient needs to have an optimal outcome for both mother and baby and what she gets. Interventions themselves as not measures of quality. Only outcomes can tell us whether we are providing high quality care.



I know this post is old. For the first time in any pregnancy this is number 5..im high risk due to an elevated level of some hormone. They didn’t tell me what it’s called. Anyway they did explain that the placenta will probably age faster than normal so I’m at risk for still birth and they will deliver at 39 weeks unless something comes up on one of the NSTs or growth scans. Anyway I know this has nothing to do with the original post but I never made a birth plan before. This time my only birth plan is just to not be pestered about breastfeeding. I felt pressured by an OB and several hospital staff members and nurses to breastfeed my last baby and I didn’t have any such plans. I had planned from the moment I knew I was pregnant to formula feed. I did eventually formula feed at 6 months but I didn’t want one day of breastfeeding and gave in anyway. This time I’m again 100 per cent opposed to using my breasts to feed my baby. I want to go back on a full dose of my seizure medicine as well as my medicine that controls complex migraines and associated nerve pain. If I make formula feeding indicated on my birth plan will that keep the high pressure breastfeeding sales people off me in the hospital? I go to a clinic for care that’s the hospital’s ob clinic (one of many) and our hospital is bfhi all the way. I know how high pressure they are because the OBs I see change from each appointment. Now I’m in their associated high risk clinic as of 28 weeks but I’m still being reminded of their breastfeeding is best baloney. I want my boobs to belong to me again. Last time I had an emotional crisis with breastfeeding. I simply want to say NO to bf and no mean no. I don’t want no to mean “what she really means is yes…She just doesn’t know it yet” no means no. This is my body. I’m hoping a clear birth plan (idc if I end up with a C-section or not. I will sign consent to all care for the baby etc) the only thing I want is to EFF and I’m hoping a birth plan that says “will only be FF and on a schedule” will be sufficient to keep the lactivists at bay.
Good luck and look after yourself. I hope your partner and family will support you at hospital to keep anyone, including breastfeeding advocates, away from you.
Maybe take some ready to feed along to give the baby so there’s no waiting while they fill out their forms.
I’ve informed every Dr that’s seen me that I will not breast feed. Even so I still got the bfhi lecture. But I have 9 weeks (give or take) until the induction as of now. They also are aware I have precipitous labors. My first was just 2 hours from the start of active labor. The second was 45 minutes from the first contraction til baby in arms. Mind he probably shouldn’t have come vaginally. I don’t know. He had mild hip dysplasia because I pushed too fast. Then my third was exactly an hour with one push and the last before this one was 1.5 hours with less than a whole push. So I’m bringing formula rtf. The unfortunate thing is that all my area hospitals (every single one within 1 hour radius) is baby friendly now! I was told many don’t offer formula at all so if you’re not going to breastfeed to keep their numbers up they will refuse it. So bring your own. I can’t wrap my head around that at all.
Anyway since I’m so fast I’m not counting on them for it at first. I’m bringing 12 rtf Similac bottles. My third was EFF after 2 months and he was the one I had the best post partum experience with. All my bf babies (love them) I struggled with sleep, feeling good about myself, emotional health, and each one ended up needing formula supplement anyway because their pediatrician didn’t like their slow growth rate. Remembering my easy time with #3 is what really led to my decision but my new diagnoses also helped me with deciding formula is best. My husband can’t stay long he will be with the other kids mostly. But I want to clearly write out that I am not following their baby friendly protocols. If she’s term I’m also not letting them toss her on me right after birth. I want her cleaned up and dressed before shes on me. Which is what I said with all the others too. They are so high pressure to keep their baby friendliness they won’t even listen to us moms. My friend gave birth at a baby friendly hospital too and I had to go demand they give her pacifiers because she wanted the baby to do something other than feed. She wanted a nap. They were being pushy. So I went and told the nurse bring formula and bring a pacifier and my friend would nap. They sighed and relented. But when it’s me and I’m tired from just giving birth I feel less in control. I wish I was a warrior for me like I was for her. Hopefully I can be stronger this time
Good luck. Keep your messages short and simple. And consistent. Maybe take a pacifier or two as well?
You sound like you have a clear plan that you have effectively communicated.
I hope it all goes well.
Thanks! I think it will go better this time. With my second baby the LC came in and actually touched my boob and shoved it in my sleepy infants mouth. I was a poor advocate then and felt very violated. I think a string of bad experiences with the breastfeeding brigade has left me actually stronger so I should be fine.
Oh I was also told to call the formula companies and ask for rtf samples and let them know the baby friendly policy will make it difficult for me and stress me out. They said the formula companies are usually more than accommodating to pregnant moms who want to have rtf formula in the hospital. I hope that is true. I’d love to gather samples.
And all the “poor outcomes” are PEOPLE! I wonder how many were hurt or killed thanks to this fetish for NCB? How many lawsuits were lost?
It also makes me really disappointed with modern medicine. If they cannot follow evidence, than who will? I am sure it was administration making these rules, but still, I wonder how many providers actually went to the mat for patients and worked to stop the rules?
No one should have to fight with a hospital to do something that is superior.
Please tell me that this will help stop all the nonsense, harmful, rules.
I am new to this site so I don’t know the policy for links but this article regarding C-section as a choice was great! http://jezebel.com/an-unnatural-birth-in-praise-of-the-caesarean-section-1644334373
“Sure: I love nature. But when nature wants you dead, fuck nature. Take medicine and science. Hell, if nature just wants you to be less comfortable than you’d like to be, fuck it. Take the epidural, and don’t feel bad about it.”
True that.
what about the routine use of pitocin for induction? If the amount is unmonitored and turned up when no progress is made, which it frequently is, and causes the baby to be in distress, that leads to a section or instrumental delivery. The forced contractions don’t give the baby access to enough oxygen during, and they don’t give the baby’s heart enough time to recover from them. That causes brain damage if baby isnt delivered quickly enough, not to mention other unnecessary risks of death or health issues to mom and baby. Or future babies if a section is performed.
That is an exact correlation between how the labor goes and the end result of birth. So yes, I would say they do have something to do with eachother.
Please provide examples of where Pitocin is ever used in an unmonitored fashion? Sounds like BS to me.
Sounds impossible to me
Actually I’m fairly certain that there’s a homebirth disaster story or two on this blog where pitocin was used. That would meet the criteria. Not exactly what Mr. Poopyhead was meaning I imagine.
Yes, I know Pitocin is used in an unmonitored fashion; in home births by lay midwives! In the hospital where I now work, Pitocin use is monitored very very closely and is turned off if the baby shows any sign of distress. The natural home birth midwives I know use Pitocin frequently and never monitor the babies at all.
Oh is that not what you were referring to, Poopy?
Sorry, birthbuddy, meant to reply to Poopy
Oh at home birth I can see that happening. Not having basic math skills and no IV pump equal recipe for disaster
Seems to me that’s exactly what they studied here – the relationship between induction and adverse outcomes in the baby (i.e. brain damage)…and found no relationship at all.
If you have scientific literature demonstrating otherwise, not fantastical anecdoctal creations, we’d love to read it.
thats laughable. see my above comments with links.
Again:
“If you have SCIENTIFIC LITERATURE demonstrating otherwise, not fantastical anecdoctal creations, we’d love to read it.”
ETA. Poopyhead.
Started to reply specifically to your comments, such as when is pitocin used without monitoring and if there was a significant number of inductions causing those complications then it would be demonstrated in this and other studies. But then I looked back at the name you signed in with and realized you’re an idiot so why bother.
You took the words right out of my mouth!
please enlighten the idiot.
Can’t be done. How about you come back with the screen name of a person not a moron, and we can go from there.
Poopyhead.
At least you acknowledge it..
“That is an exact correlation between how the labor goes and the end result of birth. ”
Load us up on some statistics then! I bet you’ve got loads of information to share with us. Information like this can’t just have been made up…
see my comment above
THAT IS NOT PROOF YOU IDIOT
Look at real papers, if you can read that well.
Your screen-name screams rational intelligence. Tell us more about how you came up with it.
Agree about the screen name–I admit mine is from a juvenile song by the Stones, but anything containing “poop” makes me think of a first grader. On the other hand, nice when Mensa members make themselves so easily identifiable. But (sigh) lord it gets tiring to hear the same lies repeated over & over.
Juvenile song by the Stones? That isn’t even possible. You’re name rocks, and is in no way immature. Silly.
http://www.baltimorebirthinjurylawyers.com/2012/10/pitocin-linked-to-childs-cerebral-palsy.html
http://www.sicklycat.com/2012/05/24/21-reasons-to-say-no-to-pitocin-according-to-manufacturer/
http://cpfamilynetwork.org/blogs/pitocin-and-its-ties-to-cerebral-palsy
http://medsfacts.com/study-PITOCIN-causing-CONGENITAL%20BRAIN%20DAMAGE.php
also heres something about the affect on BFing success from Pitocin.
http://scholarship.claremont.edu/cgi/viewcontent.cgi?article=1112&context=scripps_theses
http://www.abclawcenters.com/practice-areas/prenatal-birth-injuries/labor-and-delivery-medication-errors/pitocin-and-oxytocin
1. A jury is not a peer reviewed, replicated journal. Fail.
2. Neither are package inserts. Fail.
3. Neither is a lay person website (that acknowledges the ACOG’s approval of pitocin induction). Fail.
4. A computer algorithm says nothing of in vivo use. Fail.
5. A bachelor of arts senior thesis written by a lay person with no medical training. Fail. And LOL.
6. (below) A law firm representing birth damaged babies…I’m sure they’ve nothing to gain in this. Fail.
Really? That’s the best you’ve got Mr. Poopyhead? Not a single scholarly paper?
This reminds me of the women who print the package inserts and comments from blogs about dosing and include them in their birth plan. As in “I want this dose given and you can increase it at this amount”. Cause they google’d it.
If the package insert and the manufacturer’s statements were all that mattered Vioxx would still be on the market.
Oh those crunchy types love quoting package inserts!
Package inserts which say helpful things like ” do not take this medication if you suffer from respiratory problems” on morphine.
Which meant that my patient with end stage COPD and lung cancer was in pain and dyspnoeic because his family read that and wouldn’t let him take the oramorph that had been prescribed for symptom relief by his palliative care team.
Generally speaking, like most doctors, I have actually checked past history, allergies and current medications before recommending trying a treatment, and if I am concerned that it may have risks I will discuss them with my patient.
I recently started someone on high dose steroids, on little more than a hunch. I told them all the risks, gave them lots of information and let them know we would only go ahead if they were ok with it.
The next time I saw them I got hugs and tears.
I made the right call that time.
I know it won’t always be the right call, and I’ve thought about that before I take the decision.
Do people honestly not think that Drs weigh these decisions up?
She’s been here before and knows those are crap references.
Wait, so tricks really ARE for kids!
Too bad for the poop-meister.
Weak sauce. I can tell by the URLs that none of these are going to take me to peer-reviewed, credible articles, which is kind of important, Poopface.
Fail on the BFing article. It’s a thesis written by a lay person who is referencing people like Ina May Gaskin.
Fail on citing lawyers that make it their business to sue for “birth injury.” I wonder how many of their experts pass either the Frye or Daubert standard.
Fail on using that medsfacts link which uses a statistically insignificant sampling set to make determinations.
Fail on using that cpfamilynetwork link. that’s a blog, and it’s not saying what you seem to think it says.
Fail on sicklycat. “External Fetal Monitoring is Inaccurate.” Really now? Her other reasons are laughable and have little to no basis in scientific fact.
Please you’re making yourself look silly.
All right poop, the scenario you described sounds like you’ve read a “Sears Book” or two. Yay! You are possibly making generalizations based on what you have heard by people who obviously never experienced the benefits of a pit-drip. I appreciated my induction post-date but you don’t see me trolling NCB blogs making sweeping generalizations!
By the way your misuse of the word “correlation” annoys me to no end.
Did you even READ the post?
I’m curious, I’d-rather-post-as-guest-with-a-rude-screenname:
Are you still using this name because you are hoping your comments will be deleted because of it, allowing you to cry “censorship!”?
Dear Poopy, not sure you’ll be back to read this, or that you’ll pay much attention to it if you do, but here goes:
1. An exact correlation is 1. That means every time x happens, y happens. So, according to your logic every time pitocin is used for an induction it results in fetal distress and some kind of instrumental or surgical delivery.
2. I have had three inductions using pitocin. Often it was turned up if I wasn’t progressing. On some occasions the midwives instead had me stand up and move around a bit (sometimes it did the trick, sometimes it didn’t).
3. None of my babies experienced fetal distress. Ever.
4. None of my children were brain damaged.
5. None of my children were born by c-section.
6. Two of my children were born without epidurals (just in case you were planning on coming back at us with the other cascade of interventions).
So, not to put too fine a point on it – you are wrong.
But to be fair, and throw you a bone, I will note that my first (only post-dates induction) was delivered using the ventouse. No, he wasn’t distressed. He was 9’7″ with a remarkably large head, and the entire procedure and reasons for it were explained to me (with diagrams) before the ob proceeded.
Sincerely, mother of three beautiful children whose manner of birth pales into ever-increasing insignificance against the amazing, surprising people they are.
Oh, and 7. None of my children would speak about someone the way you have in your username, and that also has nothing to do with the way they were born.
Please read what the quality measures are… No ELECTIVE inductions prior to 39 weeks. Why not? Because there are risks related to inductions and risks related to delivering prior to 39 weeks. This is not about labor al natural. This is about a reduction in NICU admits and unnecessary c/sections…r/t failure to progress or fetal distress after being pit’d to max parameters due to an unripe cervix and down regulated oxytocin receptors.
In addition, the maternal and neonatal M&M rates… What were the controls, confounding variables and limitations? Dr. Tutuer, you pick and choose. Strengthen your arguments or change them!
What is wrong with physiologic birth? Do you distrust nature so much that you find that intervention should be rule rather than the exception?
LGA, please stick to one screen name.
“What is wrong with physiologic birth?”
It kills rather a lot of women and babies.
“Do you distrust nature so much that you find that intervention should be rule rather than the exception?”
YES.
http://mana.org/pdfs/Physiological-Birth-Consensus-Statement.pdf
This is MANA’s statement on “physiological birth”. It’s based on a bunch of misconceptions (interventions stall labor! Ect)
Correct me if I am wrong medical people, but in the context of childbirth doesn’t “elective” mean scheduled not “I am only doing this because I feel like it.” So if a woman goes in for a prenatal and it is discovered that she has something like pre-e and the doctor schedules an induction at 37 weeks in order to hopefully get the kid out before the shit hits the fan, that would be considered “elective” even though there is a pressing medical reason.
So no ELECTIVE inductions before 39 weeks will result in some dead or disabled babies and probably increase the amount of “unnecessary” c-sections as well. What is wrong with preventative medicine? Do you distrust doctors so much that you find that people should let catastrophes happen when they can be provented? Does intervention scare you so much that you would risk your or other peoples lives to avoid it?
” So if a woman goes in for a prenatal and it is discovered that she has something like pre-e and the doctor schedules an induction at 37 weeks in order to hopefully get the kid out before the shit hits the fan, that would be considered “elective” even though there is a pressing medical reason”
Maybe it depends, but where I delivered in this exact situation, it was considered a medical induction. Not sure what would be “medically necessary” if not something like pre-e. It was not subject to the 39-week rule because of pre-e diagnosis being made.
Perhaps one of the doctors here can clarify but, my point was, in my understanding, medical nescessity is completely separate from the issue of whether something is considered elective or an emergency. An emergency proceeded needs to be done now, now, now, or else someone might die. An elective proceedure can be delayed. Many elective proceedure exist to prevent emergency proceedures later on.
Considering it a “medical induction” is a separate issue. Medical induction of labor just mean a procedure was used to start your labor before it began on its own as opposed to a spontaneous induction of labor. It has nothing to do with the reasons you were induced.
Look at cholecystectomy.
If you have many episodes of biliary colic, you will be advised to have your gallbladder out. This will usually be done electively, at a later date.
Sometimes if there is a big gallstone blocking your bike duct you develop obstructive jaundice and your gallbladder has to come out then and there.
In neither case is a surgeon removing the gallbladder on a whim, both are medically indicated, but one can be pencilled in at a mutually convenient time, and the other has to happen now.
An elective induction would technically be any induction where you had time to go home, have dinner and pack a bag first.
Ok so my understanding of what is an elective procedure is correct. That is a relief.
The point is I was induced for pre-eclampsia at 37 weeks in a hospital with a ban on elective inductions before 39-weeks. My midwife couldn’t have even begun an induction if I were begging for one because of some other reason. Clearly they did not consider pre-eclampsia inductions to be “elective” and she had to document my labs and vital signs to make the case for my medically necessary induction.
That’s different from Dr. Kitty’s explanation on a “medically indicated” but not “medically necessary” induction for cholecystectomy. In gall bladder disease, the treatment isn’t delivery of the baby. In pre-eclampsia, it is.
Were you diagnosed with pre-e at 37 weeks and then immediately induced? Because if you were able to go home and come back you still had an elective induction. Chances are your hospital had a huge lists of exceptions to the 39 week rule because it would be rediculously irresponsible not to. However, when lay people and activist groups decry elective procedures without understanding what those words mean in a medical context they misinform the community and put people at risk.
If all the people decrying elective procedures before 39 weeks actual got what they say they want babies and mothers would die. That’s because they literally don’t know what they are talking about.
I agree, it’s difficult to have discussions when people don’t understand the words they are using.
Inductions are either elective or medically indicated, following the ACOG definition. That’s what the 39 week rule is based on when it comes to *inductions.* Going home and packing bags is irrelevant. I was told to go home, get my things, and go immediately to the hospital the same day my labs came in. It wasn’t an emergency, it was urgent. In the case of an emergency, a c-section is performed.
If you want to argue terminology or explain my medical care to me, would you mind showing me which published definition of “elective induction” you’re following?
Let me add, I am only arguing this point because I live in a state that has a 39-week rule, where Medicaid and the state’s largest private insurer both refuse to pay providers who perform elective deliveries before 39-weeks. I asked the DHH what evidence they were using to back their 39-week initiative and they refer me to ACOG.
If I went around accusing them of putting moms and babies of moms with pre-eclampsia (before 39-weeks) in needless danger, I would simply be wrong. The definition of “elective induction” does not apply to that list of complications in the ACOG link above.
But I wasn’t talking about the 39 week rule really. At least not how it actually practiced written and hopefully practiced because the 39 week rule is based on medical necessity (again correct me if I am wrong medical people). There are other problems with the 39 week rule that have been talked about on other places on this blog.
The OP said that she wanted it so no ELECTIVE (her caps) inductions for people before 39 weeks are done. I pointed that “elective” doesn’t mean what she thought it did. Any procedure that is not an emergency is elective and just because a procedure is elective doesn’t mean it is not necessary. Sure there are some elective procedures that are more urgent than others but something is either an emergency or it’s not. So being able to go home and pack a bag is far from irrelevent it but the entire point.
Ok, I see.
I found the Joint Commision’s definition, btw, which I guess is the one you’re using:
“elective delivery Delivery of a newborn(s) when the mother was not in active labor or presented with spontaneous ruptured membranes prior to medical induction and/or cesarean section.”
https://manual.jointcommission.org/releases/TJC2012B/AppendixCTJC.html
It’s totally different from every other definition I have seen. If that’s the case then that would explain why lay people and activists would use the term incorrectly. I do not understand why the laws crafted after the Joint Commission recommendations would have a different meaning.
Yikes. So, according to this definition…my mom who coded courtesy of HELLP Syndrome had an “elective” section. Shit, she was’t ruptured or in labor! Sure, she was DEAD, but hey, whose counting….elective it is!
Yeah, I don’t really understand that definition. There must be some rationale, I guess.
I’m so sorry about your mom.
Ah, thanks. It was really, really sad. Not to state the obvious. I should clarify that it wasn’t MY mom. A mom of a baby I took care of in the NICU. Sad. sad story.
If I went around accusing them of putting moms and babies of moms with
pre-eclampsia (before 39-weeks) in needless danger, I would simply be
wrong. The definition of “elective induction” does not apply to that
list of complications in the ACOG link above.
Sure – they would allow an induction for pre-eclampsia because it’s medically necessary, but they are still putting mothers and babies in needless danger by refusing non-medically indicated inductions before 39 weeks.
Imagine you are 38 weeks pregnant with your third child. Your first and second labors were ten hours and six hours, respectively. You live 45 minutes from the hospital in good traffic. At your 38 week appointment, you learn that you are 3-4 cm dilated and fully effaced. You could walk around pregnant for weeks, or you could have the baby any day. Who knows.
If this is 2007, before the 39-week rule became popular, your OB would probably ask you how you felt about meeting your baby today. Call your partner to bring your suitcase and get someone to pick up your kids at daycare, we can start an induction.
If this happens today, there’s nothing the doctor can do (except maybe recommend finding some place to stay in town). There’s not a single medical indication on the table. They just have to hope you make it to the hospital in time when your contractions start.
The 2007 version of events is much safer. I’d prefer it.
I can run versions of this scenario in which weather, major holidays, political conventions, sporting events, and so on are legitimate factors. It’s easy to make this scenario a lot more dangerous without piling any medical factors on.
This is why I got frustrated and asked DHH why they and all of the big insurers are now penalizing doctors for making these decisions before 39 weeks. I disagree that women with ‘soft indicators’ or other nonmedical reasons should have to wait it out until the deadline because an appeals process is too much of a hassle, or they would simply be denied an induction.
But my point was, I can’t argue for “soft indicators” and nonmedical inductions before 39 weeks by accusing them of ignoring medically necessary inductions. Because they aren’t ignoring the medically necessary inductions.
Basically, I was misunderstanding the other commenter’s point over the terminology of “elective induction.”
I am in agreement with you about the 39 week rule and its problems for women and their providers.
Ah. That makes sense. Sorry – vigorous agreement can get so weird.
One woman on a message board a couple months ago was 37 weeks with high risk pregnancy, IUGR diagnosed for a while. Had a high blood pressure reading at her MFM appointment, then another one at the regular OB’s the next day. Obviously, time for delivery. Except the nurse at MFM had not correctly recorded the blood pressure, and so the hospital could not permit it. She had to wait until Monday, for ANOTHER high blood pressure reading.
Mom and baby were OK, but that three-day delay was a stupid and unnecessary risk.
I don’t actually have an issue with early social inductions for some reasons.
If dad is a soldier going to a war zone before the due date, or there is a terminally ill relative who won’t live to see the baby if they wait til 39 weeks, I’m on board with inducing.
The odds are that a 37 or 38 weeker will be A-OK, and if they get to meet their father or grandparent, and their mum is able to attend a funeral or have an easier start to motherhood, I’d be on board with it.
Personally, I think that is holistic care, recognising that people are more than just bodies.
After being told to go straight to L&D the night that all of my paperwork met the threshhold, my midwife had to call me and cancel the induction because she misread my chart and they’d be starting it at 36w6d instead of 37 weeks. So, yeah, I had a weekend wait, too. In hindsight I am thankful because I got a little extra time and *nothing happened*, but I was not looking forward to that weekend after having some crazy high BP, seeing stars and already on bed rest for over a week by that point.
These generalized rules make sense, but it’s horrible for the women who get caught up in miserable or even deadly circumstances because the paperwork doesn’t fit for the intervention that is needed.
Even with the hospital only 15 minutes away, my contractions don’t meet the standard “5 minutes apart, hard to talk through” until within 30 minutes of delivery. I can dilate and efface “silently” all day. Makes for an easy labor and startles the L&D nurses when I’m chatting away without an epidural at 8 cm but also means I have to run to the hospital for any little twinge.
I delivered due to severe pre-eclampsia. My daughter was born by CS an hour after the decision to deliver. When I got the bill showing that insurance had paid for it, it was listed as “Elective” because it was not a crash csection. I wanted an elective CS at 38 weeks which they could not do due to the 39 week rule because I was horribly sick with vomiting but the test results came back normal. I think I could have avoided pre-e if not for that rule. my daughter and I are healthy I just hope I don’t have long term damage. some studies have shown higher risk for hypertension and shorter life expectancy after pre e.
Did your insurance company cover the entire bill (other than the usual co-pay)? I ask that because I don’t know that “elective” would apply in your case. (I was a hospital case manager for 2 years.) If you ended up paying more out of pocket, it might be worth your while to look into it.
Besides there is nothing wrong with totally elective inductions for convenience- the paper a few weeks ago with the huge numbers of women proved this.
NCBers are so hateful of modern medicine they deny moms any sort of comfort or convince, which is outrageous. Especially if you live where there is zero mat leave.
“NCBers are so hateful of modern medicine they deny moms any sort of comfort or convince, which is outrageous. ”
TRUTH
PREACH.
YES I distrust nature. “Physiologic” birth (because baby coming out w induction is what? Computer birth? Chemical birth?) would be superior IF it produced superior results.
It does not. Birth in nature KILLS and maims. MOden OB care is a huge improvement.
This is also not proof that inductions earlier wouldn’t be successful, all it measures are ones post 39 weeks. Why not go back a few and read the paper about how inductions have BETTER outcomes PERIOD.
Or are you such a nature worshipper that you cannot understand actual facts and are wedded to your NCB beliefs to the point of ignorance?
Okay, I’m going to take the shortcut of assuming that you’re talking about election WITHOUT MEDICAL INDICATION when you say “elective induction”, and proceed from there. (I’m not touching the “physiologic birth” definition with a ten-foot pole. This time.)
Delivery prior to 39 weeks is associated with a higher rate of NICU admission, however, that’s a bad reason to ban all non-medically indicated deliveries prior to that point, for several reasons, one of which is that the ban on non-medically indicated induction prior to the 39-week mark has been associated with a higher rate of stillbirth. I know which risk I prefer.
Last winter, at my sister’s 38-week OB appointment, the doctor spotted some indicators that could be early signs of placental insufficiency. My sister was ripe for induction – she had a Bishop’s score of about 11 – but the worrying indicators were too ‘soft’ for the OB to be able to send her for an immediate induction on medical grounds. They were basically waiting for an arbitrary deadline to pass OR for my sister or her baby to show signs of being critically ill. The risks of staying pregnant included fetal weight loss, placental failure, and pre-eclampsia. The risks of immediate induction were a potential brief NICU admission for transient tachypnea.
As it happened, everything went fine – my sister gave birth to a healthy, sub-six pound baby about four hours after pitocin was started, at 39 weeks exactly, and now she is going distracted trying to keep a ten-month old out of trouble. But it was only good luck that the delay didn’t imperil that happy ending. Outcomes are better when we prevent crises than they are when we insist on waiting until a crisis happens to act.
And, in short, there are risks related to expectant management as well. Risks abound. The goal is managing those risks and maximizing safety.
The practice of using interventions should be evidence-based and if evidence warrants interventions as the rule (it does), then so be it.
Hell yes, I distrust nature. Think back to the 2004 Boxing Day tsunami. It was a completely natural occurrence, generated by a completely natural shift in plate tectonics. Over 280,000 people lost their lives as a result. Nature gives life, and just as frequently ends it.
I dislike the term physiological birth. It’s judgmental against any ‘other’ birth. Though really ALL births are physiological.
Yup, without a c section my daughter would have been dead. Dying is very physiological.
SIGH…. Damn I hate it when someone tries to “sound” like they know what they are talking about.. we don’t “pit to max parameters” with an unripe cervix, brainiac.
CPOE Order: “Pitcoin: Who the fuck cares! Go Wild!”
Is that a verbal order….or a telephone read back….
LOL!! Max parameters, baby, max parameters!!
It’s a Pitocin free-for-all! Woooooot-woooot!
“CPOE Order” Just wanted to acknowledge my redundancy on that…. ; )
And also acknowledge that f-bomb may have been due to some brews at the World Series last night…Go Royals!
I’ve looked these statistics up to get an idea of how “natural friendly” a hospital was, but gave less thought to whether the numbers had anything to do with relative safety of a hospital. Implicitly, I guess the 60% c-section rate hospitals stood out to me as unsafe places, thanks to my NCB indoctrination.
It makes a lot more sense now. I remember seeing an enviably low c-section rate at one rural hospital and wondering why my hospital’s rate was so much higher. That most probably was a reflection of the hospital’s incapacity to provide routine, safe c-sections and thus only doing them when they were life or death emergencies.
It depends on the type of hospital – a major tertiary hospital in an urban with a large obstetric unit and NICU would end up with all the high-risk patients as well as all others which tends to skew their stats towards lots of surgery/intervention. A smaller hospital could well provide a safe service, but because of limitations of what they provide would only be able to take low-risk patients. Most of the time that would involve planned procedures, it would be the emergency ones they’d be seeking to avoid if at all possible because they don’t really have the facilities to deal with things like prematurity and a sick newborn. That’s why women who want VBAC sometimes have hospitals refuse them, they don’t have the facilities should things go wrong.
OT but thought this article made an interesting contrast with the “circle the wagons” mentality you get when midwives screw up: Bronx Hospital Reopens Birthing Center That Was Shut Down Due to Understaffing
I don’t know what the c section rate of my doctor or my hospital was, because it didn’t matter to me. It’s like asking how many people brought in with foot pain it ended up being a break or just a bad sprain. Other mothers needs and experiences are not mine. I had an induction (a lovely, QUALITY induction) because I was post dates with an unfavorable cervix, and a quick, easy vaginal childbirth. My doc had another woman down the hall whose attempted induction was not successful and she had a c-section. This clearly has nothing to do with the doctor OR the hospital, but rather with the woman and her individual medical needs. Thank goodness I was with a provider who could wasn’t hampered by artificial quotas regarding which medical services she should provide to her individual patients.
I didn’t ask either, about the doctor’s rate or the hospital’s. It didn’t matter to me. I was confident that, should a problem arise, my baby would be delivered in whatever way was safest for both of us. I have known women who have had unmedicated vaginal deliveries and women who have had scheduled c sections and…in the end…we’re all moms facing the same challenges. That’s the goal of birth, isn’t it: to be a mom. Does it really, really, really matter what the method of delivery is, or whether you used pain medication? No. No, it’s doesn’t matter. Not even a little bit.
I would ask, because I WANT a doc that will do a MCRS, and will not “wait and see”. I am not having a large family, so CS is superior for ME. (and I HAD a VBAC, and still think this)
I have never been as eloquent, but I have said this again and again. Cs rate should be 100% for those who need it and 0% for those who don’t. And when there is a way to predict this prior to labor everyone should be happy. Since that will never happen, we live with the best antenatal and intrapartum testing that is available, and ALWAYS err on the side of caution. Anyone judging a hospital or Ob by their cs or induction rate is an idiot. (Should have just gone with “I agree”).
That is a pretty eloquent reply for someone who claims not to be..
Thank you. I should stop now before I misspell and blame it on the autocorrect.
We say that hindsight is 20/20, but with childbirth that’s not even necessarily true. We all know stories of C-sections/inductions that should have happened and didn’t and C-sections/inductions that maybe were “unnecessary.” But honestly we can never know what things would have been like if we’d chosen Option B or C… we only know what we chose and the events that followed. So, as you said, we do our best to make informed judgments, err on the side of caution, and look at lessons learned so we can do a better job next time. And that’s all anyone can ask of a provider or patient.
Agree. We would all prefer fetal monitoring to be more sensitive with lower false positives. Same with scalp lactates/ph. Or that there will be no significant short or long term pelvic floor damage if vaginal delivery is successful. Since it’s just an educated guess, all I suggest is at least have someone in the room who is educated. Hence my support of this blog.
How about 100% for those who request it? This is my body and I don’t want to go through labor or risk tearing and infection in such a sensitive area. How I give birth should be MY choice.
I agree.
I don’t know about it now, but 6 or 7 years ago I was told to consider myself fortunate that I was given a choice between a C-section or vaginal delivery due to high risk. The OB told me some request a section and they are denied. I am hoping that policy changed or got revised. The provider who told me that interestingly enough no longer has hospital privileges.
With “need” being defined as “those who wish to have or are advised to get a c-section”? Because a lot of natural childbirth advocates harp on c-sections being “unneeded” when the baby isn’t born in major distress, inches from death, which, you know, is a terrible metric.
I vote that anyone who wasn’t actually in the room with the laboring woman and her doctor, doesn’t get to judge whether a procedure was necessary.
I’d be happy with this approach
WA state recently created a no elective inductions between 39-41 weeks as one of their quality measures (to help lower the C-section rate). My hospital doesn’t do a lot of “elective” inductions (lots of inductions, but also very high-risk population), but apparently we do enough that we didn’t meet the criteria and got dinged. Our clinical nurse educator was tell us today about this and about how the newest research shows that IOL by 41 weeks actually lowers the risk of C-section. I knew that already from reading here, but oops, your bad WA state. According to our nurse educator, the only OB on the committee that made this decision no longer actually practices. Figures. Let’s see if that quality marker goes away anytime soon.
Quality Indicators are the new black.
At least that’s what I hear…
We too are seeing fewer and fewer inductions prior to 39 weeks. Which, you know, maybe is a good thing collectively. However, now that the trend is letting women go later and later into their pregnancies….whenever we see a 40.1 + on the LD tracking shell, we in the NICU always make sure we’re ready to admit. Because about 50% of the time it happens…for a variety of reasons. Maybe it’s meconium, maybe it’s a sepsis rule out. Maybe it’s something else. But it seems like we’re getting the post-term kiddos as frequently as the pre-term kiddos, and there is something not ok with that…
50% of the time? I am guessing you have seen many term babies admitted to your NICU, but that steer away from exaggerated anecdotal evidence.
I’m actually not talking about term babies. I’m comparing pre-term and post-term. Many pre-term (late pre-term, near-term, etc. typically defined as anywhere from 35.0 – 36.6 weeks) never come to the NICU. They do fine with no help. Same with post-term babies. Sometimes they do fine, sometimes there are birth complications regarding size, length of ruptured membranes, meconium in fluids, as well as terminal meconium, etc. But sure, I’ll take back the 50% and replace it with “often.” And again, I’m talking about post-term babies, so over 41-42 weeks. Not term babies. 50% of term babies certainly do not come to the NICU. But when there’s meconium, a potential infection, decels, failure to progress, etc. – all fairly common in the post-term period, the NICU is called. And that happens often.
I just wanted to tell you I have loved reading your comments here Sally. My little guy was born at 35 weeks and he was a lucky one with no NICU stay (he didn’t pass his car seat test though, he was a car bed baby). The NICU nurse who was there in the delivery room was so amazing, reassuring me that everything they would need was either in the room or just outside the door. I will never forget her, even though the only thing we ended up needing her for was drawing blood for cultures.
Ah, thanks friend! That makes me feel good. I’m so glad your little dude never had to check in to the NICU! That’s really impressive for a 35 weeker! It’s crazy. Some 35 weekers end up intubated and needing surfactant….some just come out needing absolutely nothing at all! Glad you avoided the NICU, and I love that the nurse in your delivery was amazing. That’s how it should be. : )
He is a tough little guy-he was making the team laugh when he was a minute or two old, he kept reaching up and taking his hat off.
My own doctor couldn’t believe how well he did, her 35 weeker was in the NICU for two weeks with out of control blood sugars. Just goes to show that you can’t ever assume anything about birth or how a baby will do, so being in a setting with people who are equipped for surprisingly robust 35 weekers and term babies who need some extra care is worth it.
That’s awesome!!! Those are the best deliveries for us….when we’re completely prepared, but not at all needed!
And you nailed it. You just never know! Why not error on the side of caution? Birth is just so unpredictable!
Yeah, I always found it a bit ironic that apologies would always be offered for all those NICU attendance requests that allowed me to simply witness the beautiful moment when families meet their newest member … quietly “holding space” in the corner. Best part of the job hands down!
Seriously! No apologies needed! We love false alarms! : )
I had 2 NICU babies, both had really nasty, and rare, blood incompatibility issues. I guess these factors usually aren’t so serious (Big C, little e, and another I can’t remember.) Someone has to be that 5% right?
My first was a healthy, full term 9.5# baby (via CS), but yellow as could be. He was there nearly 6 weeks! Blood transfusions, lights, some med that starts with IG, the whole nine yards. He left at 14#- one of the NICU nurses asked me if my baby atte one of the other babies, LOL.
The second one (VBAC) had the same HDN, but was also a 33 weeker, because of extreme funneling in cervix that required cerclage at 19 weeks (yikes!). She still got the meds, but only 1 transfusion.
I was monitored well so she got and whatever else. Too many details! She did come out breathing and never had those issues. She latched onto the boob the 3rd say out, though she wasn’t strong enough to get much milk (at 2.5 she is still a boob junkie).
LOVE YOU NICU NURSES
Wow! Sounds like you know your way around the NICU! I bet the nurses loved you…sounds like you have a great sense of humor and were pretty go-with-the-flow. So, I’m guessing your two babies were Coombs positive…making them high risk for hyperbilirubin. Good times! Good times. Glad everyone rocked out and is doing well. So glad your experience in the NICU was good…we love NICU parents!!!
Well we know that term elective induction (39/40 weeks), as opposed to expectant management to 40-41-42 weeks, reduces the risk of having a C-section. If it’s easier for a baby to get out on his own if he’s born at term, makes sense to me that he would also have fewer complications than at post-term.
Pssssst….So, today, 100% of post-term babies came to the NICU. One was a meconium aspiration…not pretty. The next became tachypeic two hours after birth…breathing between 80 – 110 a minute. CBC showed a 0.8 left shift.
Sure, only two babies. But it’s still 100%.
Boom.
I would rather a healthy baby a bit early with a bit of issues, than a sick one post dates.
With amnio, this is really not a worthwhile risk.
Amen, sister!
Not to mention there is that incentive of extra reimbursement if the rates are kept low-if the hospital accepts DSHS (or whatever pregnancy Medicaid is called now in WA).
This is why Australia’s “towards normal birth” policy is such crap. It is politically and financially motivated without any medical basis. Lowering inductions AND c-sections will not result in better outcomes. Maybe at the extremes, but not for most. It is like the old WHO optimum cs rate of 15%. A meaningless number. find the country/ hospital/group with the best outcomes, and look at their rates of cs and induction. Not the other way around.
You know where the 15% limit makes sense? Countries with very limited medical facilities, where women sometimes die from c-section complications, may not have any way to limit their family size, and may not have decent medical help for the next birth.
And if there is any policy goal, it should be towards making the options (and subsequent better outcomes) available in rich areas available in poor areas, NOT in limiting the options in rich areas to what is barely available in poor areas.
Dang, I’d love to know what the r-squared values are on those scatterplots. To the naked eye, they all look like zeroes.
There’s a very, very slight negative correlation on the bottom right (neonatal morbidity vs c-section right), as in, more sections, lower morbidity, although it will be even less if you throw out that outlier
Why not measure actual maternal morbidity?
Mothers requiring post partum IV antibiotics, or manual removal of placenta, or blood transfusion.
I think CS and induction rates could be quite useful when choosing a practice. Look for high rates, and it’s likely you’ve found a practice that prioritises patient safety above unscientific ideology. Sounds good to me.
Only to a point. It’s a curve, not a diagonal straight relationship. Rates at the extremes are likely to reflect either patient selection or bad practice.
Somebody did a study where they attempted to adjust for ALL maternal risk factors, and then compare cesarean rates and neonatal outcomes between hospitals.
They found that most hospitals had an “adjusted” cesarean rate around 5%, and that hospitals with higher or lower rates had poorer outcomes.
I know that if knew I was going to need a cesarean, I would like to find a doctor with a higher cesarean rate. The more experience they have with the procedure I need, the better.
A few years ago I thought I’d struck gold when I found a provider in our area that had a C-section rate around 15%… until I found out through the grapevine (a friend of a friend works in L&D at the hospital where this OB delivers) that the doctor has a reputation for botched Cesareans. She avoids them because she’s uncomfortable with them, hence her low surgical rate. At the time I was still deep enough in the woo that I desperately wanted to avoid an induction or C-section, but I had “woken up” enough to know that if I DID need surgery, I wanted someone who was competent.
My doctor for one of my pregnancies had a cesarean rate of 8%, while the rate at the local hospital was close to 50%. That looks bad, but we were in a very rural area with a lot of obesity and poor people and limited obstetric emergency options.
My doctor had such a low cesarean rate because he was actually a GP. He referred likely cesarean deliveries to the one OB in town as early in pregnancy as possible, so only those needing urgent cesareans counted towards his rate (although technically his rate was zero, as the OB actually did the surgery).
Exactly – there are a great many factors that push a rate up or down, and the weight of each of those factors varies from one provider to another. It’s absurd to assume that we can get an idea of whether or not a doctor is *good* or *bad* just by looking at one metric.
Look at regional areas in states and you’ll find a teaching hospital with a great NICU and several level II or level I hospitals who transfer all high risk patients less than 34-32 weeks. This will obviously lower the CS rate of smaller hospitals and raise the high risk patients and CS rates at bigger hospitals. Or at least decrease the expertise of the smaller hospitals physicians when a critical patient come through the ER and have no time to transfer.
My feeling is that in general, if there are different ways to an outcome, go with whatever the practitioner does the most. They will be good at it and familiar with any complications and prepared for them.
If your OB is conservative and does c-sections at the drop of a hat, go with that. If your OB prefers to avoid c-section and has developed a particular expertise with forceps, go with that.
That’s assuming you can be sure that the practitioner has met a basic good-enough standard. (An OB is good-enough. A CPM is not.)
Don’t get it. Nope. Not at all. No can do. The whole point of birth is to HAVE A HEALTHY BABY, hence why it’s called HAVING A BABY. who gives an ever loving fuck what it takes to achieve that? How does a C section represent a worse “experience” than having a dead baby? Or worse yet, a dead baby and a dead mother? Both are genuine possibilities. How is it that we’ve forgotten that both a dead baby and a dead mother were common occurrences less than a century ago, specifically because we didn’t have the life-saving “interventions” we now have? WHAT IS WRONG WITH THESE FUCKING PEOPLE?!!!
Honestly, my experience is that a lot of the people who prioritize the “experience” are spoiled. A “bad experience” is the worst thing that can happen in their world, because they frequently haven’t experienced REAL difficulty. I had a hellacious pregnancy and birth with my oldest, and would do it again in a heartbeat to have my stillborn son back.
“I had a hellacious pregnancy and birth with my oldest, and would do it again in a heartbeat to have my stillborn son back.”
*hugs*
I’m not spoiled, have lived a life of hard and easy times, and I still value my birth experience. Not for the bragging rights, but for my introduction as a new person- a mom. For my psychological, physical, spiritual, and sexual health. It matters a lot more than people think.
And btw- of course a healthy baby matters at the end, but so does a mother’s mental and physical state. We all know we would all do everything for our babies, that we sacrifice so much for our children. And mothers who choose any type of birth very much believe they are doing just that. Just bc a mom had a baby, doesnt mean she should suck up her feelings of whatever her experience was and either hide them in shame or brush them off as no big deal comparatively.
It would be like telling a mother whose baby died to get over it when she finally does have a healthy/live baby. One thing does not negate the other.
My condolences,btw. Hugs.
What kind of mental state might a mother be in as she plans her newborn’s funeral? Or arranges 24 hour care for a brain damaged baby?
“It would be like telling a mother whose baby died to get over it”.
That is exactly what NCB do.
NO ONE SAYS MOMS MENTAL STATE DOES NOT MATTER. Of course it does, as does her comfort (hence epidurals on request), and her integrity and autonomy!
Talk about straw man arguments!
You’re my favourite with your original, well thought out name. And just when I think you couldn’t be more stupid, vicious and shallow, up you pop with a remark like this.
And you still talk about your birth experience, you becoming a mom, and your various states of health, still no mention of the other human involved, that is the baby you conjured up.
Though I think you may be growing, I see in your reply to yourself below you finally, having yet again pushed your tedious boorish nonsense, managed a belated and offhand acknowledgement of Midtown Parent’s loss.
I totally valued the birth experience, and did everything I could to make it perfect for ME. I think most moms agree with this- who doesn’t want to be comfortable, respected, and even enjoy it if possible?
But that is NOT the point here.
The point we are trying to make is that making your experience wonderful is what you worry about AFTER all of the critical safety issues are considered. This is because a fantastic experience will not make up for your baby dying or getting brain damaged, or losing your uterus, or having other severe health issues.
Making choices in order to get that positive experience, with the trade off of (often extremely) increased risk, makes no sense to most of us. I know some moms make those choices, but most only do because they really don’t think there IS increased risk! Rarely do I hear a mom say “yeah, HB is more dangerous, but its worth it!”
Not that you can’t have both, if all goes well. The hospital I had DD in was amazing. But this idea that we are owned a great experience is kind of nuts, when you consider the history of birth, and the risk you take on to do it.
No one knows…
And women are still left guessing, essentially, when it comes time to choose a practice & setting. I would rather have meaningful numbers, but I *need* numbers & I feel like if men gave birth we would already have them.
If men gave birth the standard would be a c-section at 38 weeks, with a fully staffed nursery to take care of the newborns for several days. Breastfeeding wouldn’t exist. The painkillers freely given to postpartum dads would be amazing.
And there sure as hell wouldn’t be anyone denying or discouraging pain management based on myths perpetrated on dumb birth blogs.
The worst blog post I ever read was from a woman who was apparently passing out leaflets at some community fair (???) about NCB & the wonders of drug-free delivery. Supposedly, she got comments like, “But I’m all about the drugs!” from smiling women, which made her so angry she had to go–post! The main gist of her argument was “Think of what those drugs do to your poor newborn!” I think at one point she acknowledges that sure, drs say that epidurals have little to no effect on the newborn, but (cackle) what do you expect them say? I’m sure that back when the only pain relief option was morphine & its analogs they were some buzzed groggy newborns out there…but she continued w. her argument-by-lack of evidence. Does anyone remember who wrote that tripe? She also wrote a birth plan to the effect of “If I need to transfer, while I am in the hospital communicate everything through my hubby or doula & don’t talk to me or touch me.” I remember thinking, “It’s your child’s life, not an opportunity for you to throw a tantrum, dear.” I’m sure the nurses were just thrilled to have such a lovely patient & drew straws for the privilege of approaching her & saying, “I just need to take you–”
“NOOOOOOOOOOO!”
Change it to 39 weeks and PCA epidural placed at the hint of pain ( about 20 weeks) and I’ll agree
Postpartum doulas would be free for overnight and evening shifts at home for the first six weeks
That is in fact what I did when both of my grandchildren were born — I went on “night shift” [something I have a great deal of experience with], and slept during the mornings so that my daughter could get to sleep from 10 p.m. to 5 a.m. at least. She pumped enough milk for me to do the middle-of-the-night feed from a bottle, and didn’t have to wait for hours for a colicky baby to settle down.
You are amazing. I wish I could have had that. I was taking care of my own mom when I had my first child, she had a stroke. She had a lot of helpful tips about baby soothing and breastfeeding and we spent a lot of time together so it was a blessing for both of us.
Of course we would. We would have anything you could ever deem needed, or even wanted, if MEN need it. We are second class citizens.
This is a depressing fact about quality measures in hospital care: most of them are easily-measurable things that are seized upon by management staff just to show that we are monitoring ‘quality’ which becomes a commodity, an attribute to tout to the hospital’s parent system and to insurers. The Baby Friendly designation is one such attribute. C/S rates are another. We recently got dinged during our ‘time out’ in the c/s room because the doctors were not reading from the consent form when they named the patient and the procedure! I’m getting quite the rep at department meetings for bitching about silly measures.
My latest battle was over the inclusion of third and fourth-degree lacerations as a quality indicator. I said it was absurd, and insisted that it not be tracked. Our Risk Manager said something along the lines of all the other hospitals doing it. I asked her if she would like our doctors to do more c/s as a way of preventing these lacerations….and that was that.
Touche’!
Inappropriate targets and KPIs can cause more harm than good.
Why don’t you want to track lacerations? Wouldn’t it be useful to see the tradeoff? If you want to be able to argue for less pressure to reduce c-section, don’t you want the data?
Wouldn’t an individual practitioner be relieved at the option to get points back with reduced laceration, that they had given up by performing a c-section?
See my reply to huh? above.
Thanks!
Why do you think lacerations don’t matter?
I think what she’s getting at may be that these lacerations have more to do with the size of the baby and the physiology of the mother. Neither of these things are within an OB’s control.
About the only thing an OB can do is perform a c/s if it looks like the mother is at risk of a severe tear. So if you track both severe tearing and c-sections, you will never get an “ideal” rate of both.
It’s not that they don’t matter. Of course they matter. They just aren’t a quality measure. I review scores of charts. Every OB and CNM occasionally has one; the anus and rectum are very much in harm’s way and occasionally are injured. There’s some typical maneuvers you can do to reduce injury but injury will happen. Now a true quality measure is the rate at which they are recognized, repaired appropriately, and heal well. THAT is a quality measure.
This is one of the most sensible things I’ve ever read. Can we start a write-in campaign for Obama to nominate you as Surgeon General, or at least get you a cushy job at WHO? 🙂 One of my dedicated NCB SILs’ OB told her that he felt 3 & 4th degree tears were “too high a price” just to avoid a c-section–not sure if many or even a few docs agree with that, but that’s what he apparently said. She found a midwife instead and homebirthed, which she had been planning to do anyway (she just wasn’t planning to have even a midwife)–and she ended up she had to go to the hospital and get her 3rd-degree lac repaired. To top it off, she now has problems they want to fix surgically, but is afraid of transvaginal mesh b/c of “what you hear about it on TV.” They are into NCB for religious reasons, not ideological ones, which I guess might make it easier to swallow when things go wrong, though I imagine the pain is the same.
I WISH Addie was in charge! SHe is the most awesome OB ever and would do a lot for women’s health.
Oh, I hope people don’t think I was sarcastic–I was deadly serious! I really do wish she was in charge, b/c I think if a lot of women heard good, intelligent, arguments against the NCB gospel, they would not only be more supportive of each other but more forgiving of themselves, and you can’t put a price on that.
So, if I understand correctly, the best way to determine quality is measure maternal and perinatal morbidity and mortality, but also control for populations?
if you are going to measures outcomes, you need to risk adjust the data if you want to compare across institutions. If you only want to use the data internally, you can avoid risk adjustment and do comparisons over time (like run charts etc) but only if you are reasonably sure that your served population and their characteristics are stable.
Even process measures, we now understand, need risk adjustment. For example, sicker patients are less likely (appropriately so) to get some testing or preventative medicine. For example, if you have metastatic cancer and a shortened life expectancy from that, do you really need the statin to marginally lower your chance of a heart attack?
I think the best combo is to measure outcome and then also measure what the known or suspected key drivers are (usually processes) and see if you can establish a linkage within your environment. For example, I could measure the labour epidural failure rate and then the key drivers could be things like time of year (new residents with less experience), time of day (less resources to troubleshoot at night), the use of opioid and local anesthetic solutions vs only local anesthetic, the concentration of local anesthetic used, the rate of infusion, the proportion of women that get PCEAs, the dilation at epidural placement (bc I would wonder if epis placed close to transition would be more difficult bc of squirmy or work less well because no time to fix them), the use of US for landmarking etc.
That makes sense. I was thinking of hospitals that have a lot of high-risk patients vs. ones that have low risk patients. Clearly, they can’t really be directly compared, because you would expect worse outcome in the high risk population. Some of the NCB types don’t seem to understand that though, and see only the Csection rate (for example)–OMG, it’s 45%!! Yeah, but its a major teaching hospital with a fertility center, a level 3 NICU, and a top-notch MFM team.
I would hope that anyone who uses stats to adjust policy thinks like you, and accounts for the real reasons why things might be the way they are. (re: your epidural failure rate example) You can’t control when the new residents arrive, but maybe you can see that they have more supervision or something like that, rather than say, decide that epidurals should be with-held during July or whenever the residents show up.
The number one thing you need to know in the UK health service?
Under no circumstances get sick on the first Wednesday in August, which is changeover day.
You’ll have a medical team of complete strangers, all starting new posts except for the boss, and the junior members will be complete rookies.
Frankly, it would be a miracle if the death rate DIDN’T spike.
Actually I have heard it said the accidents for residents tend to start 3-4 months later. In the first months it’s known they are brand new and there is a ton of oversight. As people become more accustomed and both attendings and residents become more confident in their skills they tend to let go more. That critical point where you are good enough that people trust you and you trust yourself, but still not good enough to really fly solo or as solo as you are being allowed to at least. The real issue is being able to determine with 100% accuracy what level of autonomy each individual is ready for.