The increased risk of death and serious injury at American homebirth is well established and a remarkably robust finding across multiple studies, including:
Grünebaum A, McCullough LB, Sapra KJ, et al. Early and Total Neonatal Mortality in Relation to Birth Setting in the United States, 2006-2009. Am J Obstet Gynecol. 2014 Mar 21. pii: S0002-9378(14)00275-0. doi: 10.1016/j.ajog.2014.03.047.
Cheng YW, Snowden JM, King TL, Caughey AB. Selected perinatal outcomes associated with planned home births in the United States. Am J Obstet Gynecol. 2013; 209: 325.e1-8.
Grünebaum A, McCullough LB, Sapra KJ, et al. Apgar Score of Zero at Five Minutes and Neonatal Seizures or Serious Neurologic Dysfunction in Relation to Birth Setting. Am J Obstet Gynecol. 2013; 209: e1-323. e6
Wasden, S., Perlman, J., Chasen, S., and Lipkind, H. 506: Home birth and risk of neonatal hypoxic ischemic encephalopathy. Am J Obstet Gynecol. 2014; 210: S25
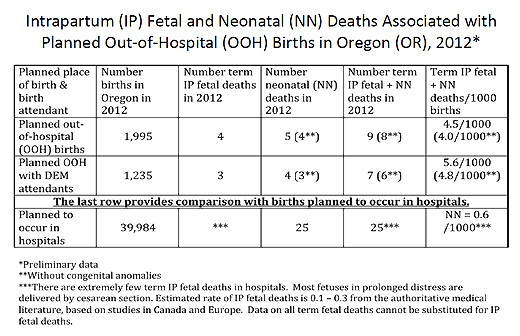
The most remarkable finding is the analysis of Oregon data from 2012 by Judith Rooks, CNM, MPH demonstrating the planned homebirth with a licensed (CPM, LM, DEM) midwife has a perinatal death rate 800% higher than comparable risk hospital birth.
Even the data from the Midwives Alliance of North America survey of their members (Cheyney M, Bovbjerg M, Everson C, Gordon W, Hannibal D, Vedam S. Outcomes of Care for 16,924 Planned Home Births in the United States: The Midwives Alliance of North America Statistics Project, 2004 to 2009. J Midwifery Womens Health. 2014; 59: 17-27) shows that homebirth increases the risk of perinatal death by 450%.
Why do so many babies die at homebirth? A new paper Perinatal Risks of Planned Home Births in the United States by Grunebaum et al. provides answers.
Data from the United States (US) Centers for Disease Control’s National Center for Health Statistics birth certificate data files from 2010-2012 were utilized to analyze the frequency of certain perinatal risk factors which were associated with planned midwife-attended home births in the United States and compare them with deliveries performed in the hospital by certified nurse midwives (CNM). Home birth deliveries attended by “others” were excluded; only planned home births attended by midwives were included. Hospital deliveries attended by certified nurse midwives served as the reference. Perinatal risk factors were those established by ACOG and AAP.
What did the authors find?
Twins:
… 1 in 156 (0.64%) of midwife-attended planned home births were twin pregnancies, even though ACOG considers twins a contraindication for home births, as there is no adequate fetal monitoring, no experienced team, and no ultrasound available in home births. Studies on safety of home births from Canada, England, and the Netherlands excluded twins as candidates for home birth because of increased risks..
Breech:
… 1 in 135 (0.74%) of planned home births attended by midwives were vaginal breech deliveries. Breech vaginal birth is associated with significantly increased risks… Azria et al. recommended that a trial for vaginal births in breech presentations should be attempted only with continuous electronic fetal heart rate monitoring (EFM) and presence of ultrasound during labor and delivery. Neither EFM nor ultrasound is available in home births. Janssen from Canada and the Home birth in England Study excluded breech presentations from their home birth eligibility requirements. Therefore it is not surprising that the Midwives Alliance of North America (MANA) study of planned home births, reported an intrapartum death rate of 13.51/1,000 and a 9.16/1,000 neonatal mortality rate in breech presentations.19 When compared to the neonatal death rates from hospital deliveries these adverse neonatal outcomes are significantly increased
Postterm:
ACOG and AAP criteria for home births specifically exclude pregnancies ≥41 weeks from their home birth eligibility. In this study, 28.19% of home births were ≥41 weeks. Postterm pregnancies are associated with multiple, well-known complications, such as labor dystocia, increased perinatal mortality rate, low umbilical artery pH levels at delivery, low 5-minute Apgar scores, postmaturity syndrome, fetal distress, cephalo-pelvic disproportion, postpartum hemorrhage, and increased risk of neonatal death within the first year of life.
Attempted vaginal birth after C-section (VBAC):
A trial of labor after prior cesarean delivery (TOLAC) is associated with a greater perinatal risk than is elective repeat cesarean delivery without labor. TOLACs have an overall small but significantly increased risk of uterine rupture with often catastrophic consequences to mother and/or fetus.22,23 This study showed that nearly 1 in 23 (4.4%) of midwife-attended home births (n=2,463, 4.4%) had a home VBAC in spite of the fact that ACOG considers prior cesarean section an absolute contraindication to planned home birth… The recent MANA study showed a very high 2.85/1,000 intrapartum fetal death rate with VBACs.
In other words, babies die because American homebirth midwives ignore the risk guidelines accepted by ACOG, the American Academy of Pediatrics, Dutch midwives, British midwives and Canadian midwives. What’s the difference between American homebirth midwives and every other provider who accepts the risk guidelines? American homebirth midwives aren’t real midwives. They lack the education and training of ALL other midwives in the industrialized world and they are ineligible for licensure in ALL other first world countries. American homebirth midwives are lay “birth junkies” who made up their own credential and awarded it to themselves in order to trick American women into thinking they are healthcare providers.
American homebirth midwives are frauds and ignore the safety guidelines accepted by midwives and obstetricians around the world. It is hardly surprising then that so many babies die at American homebirth.