Homebirth advocates exult that the proportion of planned homebirths in the US has been rising from miniscule to slightly more than miniscule. Too bad they never point out the endless stream of preventable homebirth deaths that result.
I noted earlier this month that there are so many homebirth deaths that I can barely keep track. There was an additional homebirth death just this past weekend.
First, though, I’d like to update the information on a death that I mentioned in the above post:
A baby who died in Phoenix last week whose mother, a doula, had a previous HBAC. I have not been able to establish whether the caregiver knew that the baby was dead before birth or was not expecting it.
It turns out that I had written about the mother before. She runs the Big Baby Project, which I wrote about here.
In a bio for a this piece and the follow up piece she wrote for a birth website, Cherise Sant is described as:
…Mother, Doula, Childbirth Educator, Placenta Crafter, and Creator of the marvelous “Big Baby Project” (a website full of empowering vaginal births of babies 9 lbs and over).
Sant is a purveyor of the standard homebirth trope.
Disappointment with her first birth:
I had resisted an induction but eventually caved to the pressure I was receiving from my obstetrician. The ultimate result was a healthy baby boy born via cesarean and my broken heart and body.
A successful hospital VBAC:
My second birth was an empowering vaginal birth in the hospital, but I was met with mistrust, abandonment and even violence though I had carefully chosen my provider and a “natural birth friendly” hospital.
Then the successful HBAC and total lack of awareness that the baby was possibly borderline IUGR:
We had a boy! As I’d pulled him up, I immediately could tell that he was little!! My smallest baby for sure, and yes he weighed in at 5 pounds, 15.9 oz. Later I would marvel that I changed course on a path to VBAC and didn’t have planned cesareans at 39 weeks. I couldn’t imagine how small and fragile he would have been 2 ½ weeks prior.
But if he was IUGR, he was not getting stronger in the two weeks after 39 weeks. He was struggling to survive despite a placenta that was depriving him of adequate oxygen and nutrients.
Sant had dodged a bullet, but she didn’t realize it.
This time around she was not so lucky. This baby was stillborn.
According to a post left on the Big Baby Project Facebook page, the baby died during labor:
This wonderful woman, Cherise Sant, who has been a support and strength to many, including this community, recently lost her sweet babe during childbirth. Please help them if you can. Look at her photos and let their story touch you. Spread the love!
Cherise Sant is a doula who headed up the Big Baby Project though she hadn’t had a big baby herself, she spent countless hours helping all women to have a wonderful birthing experience, no matter how big their baby was measuring.
She is very involved in the birthing and natural living communities.
She has been a strength and inspiration. I hope we can reach out to her now!
In other words, she inspired other women to play Russian Roulette by holding a figurative gun to their babies’ heads just like she did.
Inevitably, there is the obligatory plea for money accompanied by a heartbreakingly beautiful picture of a stillborn baby.
This baby lost his mother’s game of Russian Roulette. Perhaps his death may serve as an inspiration to women contemplating homebirth not to play Russian roulette with their babies’ lives.
*****
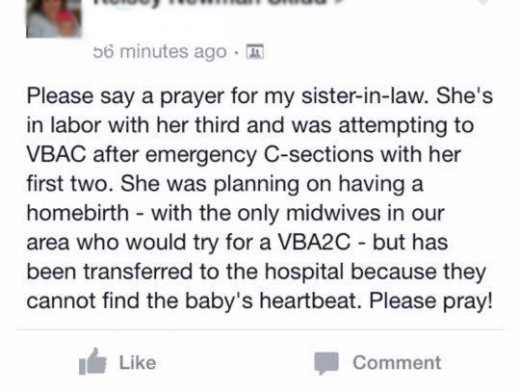
But, tragically that’s not all for March.
A Connecticut mother played Russian Roulette and her baby lost, too.
She was laboring at home at 41 1/2 weeks.
Her uterus ruptured and the baby died. The mother survived.
Her “midwives” are a CPM and a lay midwife.
This will be yet another opportunity for CPMs to practice “letting go.” It couldn’t be letting go of babies lives could it? It could.
As Lana Muniz writes:
Homebirth midwives “value the art of letting go.” Letting go of what, exactly? The lives of babies born at homebirths.
We know this because it’s written in the MANA Statement of Values and Ethics right on their website,
“… We value the art of letting go and acknowledge death and loss as possible outcomes of pregnancy and birth.”
It’s a disturbing statement coming from an organization that claims homebirth is safe, even though it’s 4 times more deadly than hospital birth.
Muniz provided chilling quotes from Professional Ethics in Midwifery Practice by Illysa Foster and Jon Lasser:
We value the acceptance of death as a possible outcome of birth. We value our focus as supporting life rather than avoiding death…
We place the emphasis of our care on supporting life (preventive measures, good nutrition, emotional health, etc.) and not pathology, diagnosis, treatment of problems, and heroic solutions in an attempt to preserve life at any cost of quality.
In other words, they place the emphasis on what they can provide (and bill for) and NOT diagnosis, NOT treatment of problems, NOT heroic solutions (all things they cannot provide and therefore cannot profit from).
They can provide preventive measures for playing Russian Roulette (nutrition, emotional health), but if you’re the unlucky mother with a bullet in the chamber when she figuratively fires into her baby, they not only can’t fix it, but, apparently, they don’t even think it is worth trying.
This is what “ethics” looks like in the world of homebirth midwifery. It’s a farce, just as their education and training is a farce.
*****
If you’re a mother thinking about homebirth, think again.
Do you really want to play Russian Roulette with your baby’s life? No doubt you think this couldn’t happen to you, but, then these mothers thought that too and now they are burying their babies.