Natural childbirth and homebirth advocates love to bemoan the “cascade of interventions.” Their theory is that every intervention leads to more interventions until finally a C-section is necessary. The implication is that if the first intervention had been withheld, the mother would have gone on to have an uncomplicated vaginal delivery of a healthy baby. But like so much of natural childbirth and homebirth advocacy, the dreaded cascade of interventions is made up crap, designed to demonize tests and procedures that the natural childbirth industry cannot provide or profit from.
In fact, in many cases, the opposite is true. Many interventions make it LESS likely that a mother will have a C-section, not more. For example, there is a growing body of evidence that induction of labor leads to a LOWER C-section rate than awaiting spontaneous labor. A large, comprehensive study just published in the Canadian Medical Association Journal provides the most compelling evidence yet that induction lowers the risk of C-section.
The study is Use of labour induction and risk of cesarean delivery: a systematic review and meta-analysis by Mishanina et al.
The authors explain:
Although induction of labour has been criticized for an associated increased risk of cesarean delivery, recent studies have shown that there are fewer cesarean deliveries with induction than without it. However, the findings have not had much impact on practice, in part because the systematic reviews investigated subsets of induction and included few randomized controlled trials (RCTs), and because observational data in a cohort study had risk of confounding. Consumer organizations, guidelines and textbooks have given contradictory information about cesarean risk, which can lead to confusion over decision-making, particularly given a desire to support normal birth in the face of increasing cesarean rates worldwide…
How did the authors investigate the issue?
We searched 6 electronic databases for relevant articles published through April 2012 to identify randomized controlled trials (RCTs) in which labour induction was compared with placebo or expectant management among women with a viable singleton pregnancy. We assessed risk of bias and obtained data on rates of cesarean delivery. We used regression analysis techniques to explore the effect of patient characteristics, induction methods and study quality on risk of cesarean delivery.
The literature review led to 157 papers encompassing 31,085 women.
What did they find?
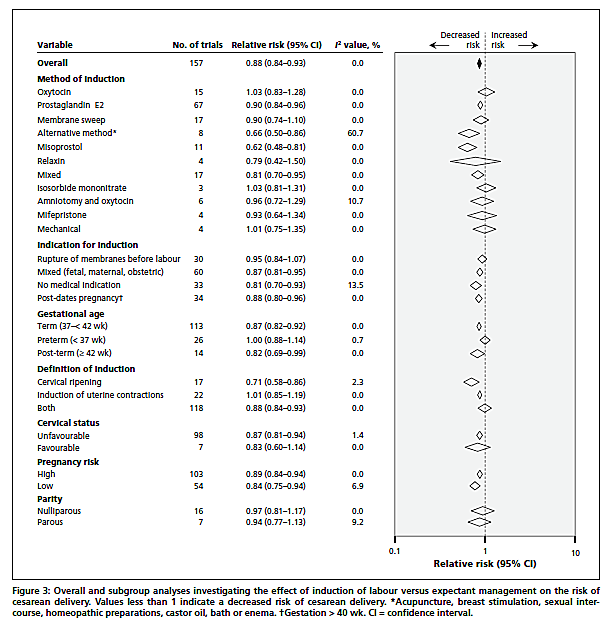
Overall, … the risk of cesarean delivery was lower with labour induction than with expectant management (pooled RR 0.88, 95% CI 0.84–0.93)…
In the subgroup analysis by method of induction, 4 methods were associated with a significant reduction in risk of cesarean delivery: prostaglandin E2 (RR 0.90, 95% CI 0.84–0.96; I2 = 0%), misoprostol (RR 0.62, 95% CI 0.48–0.81; I2 = 0%), alternative method (RR 0.66, 95% CI 0.50–0.86; I2 = 60.7%) and mixed method (RR 0.81, 95% CI 0.70–0.95; I2 = 0%).
Subgroup analysis by indication for induction showed a universal reduction in risk of cesarean delivery. Induction without a medical indication provided was associated with risk reduction of 19% (RR 0.81, 95% CI 0.70–0.93; I2 = 13.5%). When we looked at risk of cesarean delivery by gestational age, we found statistically significant reductions in risk with labour induction in term and post-term pregnancies, but not in preterm pregnancies.
In the analysis by definition of induction, risk of cesarean delivery was significantly lower when the definition included cervical ripening alone or combined with stimulation of uterine contractions than when it included uterine stimulation alone. The analysis by cervical status showed a 13% reduction in risk of cesarean delivery if the cervix was unfavourable at induction (RR 0.87, 95% CI 0.81–0.94; I2 = 1.4%) and no difference in risk if the cervix was favourable (RR 0.83, 95% CI 0.60–1.14; I2 = 0%).
The risk of cesarean delivery was reduced in both high- and low-risk pregnancies.
In other words, induction lowered C-section rates for nearly every possible indication including NO indication, using every one of the most common agents, for both term and postterm pregnancies, in both high and low risk pregnancies, and even if cervical status was unfavorable.
The authors include a forest plot that graphically illustrates the results:
In addition, outcomes were better with induction:
Analysis of adverse outcomes showed a lower risk of fetal death and admission to neonatal intensive care unit associated with labour induction than with expectant management. No impact on maternal death was shown.
The authors conclude:
Our meta-analysis has provided a robust answer to the disputed question of risk of cesarean delivery associated with induction of labour. Women whose labour was induced were less likely than those managed expectantly to have a cesarean delivery. In addition, the risk of fetal death and admission to neonatal intensive care unit were decreased in the induction group. Our findings have implications for guidelines and the practice of obstetrics, and are reassuring for mothers, midwifes and obstetricians.
So it seems that if you want to reduce your risk of C-section, one of the most effective things that you can do is to have an induction of labor.
Ironic, no?