I’ve often remarked that no sooner do I write a post about some aspect of the natural childbirth industry than advocates leap to validate my concerns and demonstrate the truth of my warnings.
Today Rebecca Dekker demonstrates the seductive marketing tactics of the natural childbirth industry.
Her latest piece is What is the Evidence for Inducing Labor if Your Water Breaks at Term?, which, as it typical in the natural childbirth industry, an alternate world of internal legitimacy, was immediately trumpeted by another industry outlet, Lamaze International’s Science and Sensibility.
In a piece nearly 10,000 words long, Dekker and associates break no new ground, come up with no new recommendations, but act as if they’ve reinvented the wheel.
For perspective, let me tell you how prolonged rupture of membranes was managed 30 years ago when I started my training:
If a woman at term presented with ruptured membranes but not in labor, she was assessed for fetal well being (using the fetal monitor), maternal well being (including fever) and risk factors. No vaginal exams were done; occasionally a sterile speculum exam was performed. In the absence risk factors, the woman was advised to wait 24 hours and then return for possible induction of labor since the risk of an neonatal sepsis (severe infection of the newborn) begins to rise after membranes have been ruptured for more than 24 hours.
What did Dekker and associates recommend after their 10,000 word review? EXACTLY THE SAME THING!
Evidence shows that in women who meet certain criteria (single baby, head-first position, clear fluid, no fever or signs of infection in mother or baby, negative Group B Strep test), waiting for labor to start on its own for up to 2-3 days is as safe for the baby as inducing labor right away, although the mother is more likely to get an infection herself.
So what’s the big deal? Why the hoopla, the avalanche of words, the charts and lists?
That’s all part of the seductive marketing tactics of the natural childbirth industry that Dekker is so helpfully illustrating for us.
To wit:
1. Never forget that natural childbirth is an industry
Dekker is constantly branding and constantly selling. And she doesn’t let you forget it.
Through December 1 only, you can download a printer-friendly PDF of this entire article, plus a 52-page annotated bibliography PDF, for FREE!! Included with your download is copyright permission to print and share the blog article PDF with anyone you like– friends, health care providers, coworkers, clients! The cost of these two PDFs is “pay what you want,” meaning that you can download them for free, or you can pay what you feel is the value of these materials (suggested value = $5-10).
All flyers preview
Those who give $25 will receive a high-resolution of these 8.5 by 11 inch PROM flyers to print and share with anyone you like!
If you want to purchase the PDFs, I have a special “thank you” for those of you who pay $15 or more. In addition to the printer-friendly PDF and the annotated bibliography, you will get access to an online quiz about PROM that you can take to earn a continuing education certificate for one nursing contact hour!! Nursing contact hours are accepted by most doula, childbirth educator, and some midwifery organizations (check with your certifying organization to see if they accept nursing contact hours.)
Finally, for those of you who pay $25 or more for the materials, you will get everything listed above– the printer-friendly PDF, annotated bibliography, quiz plus contact hour, PLUS four colorful 8.5 x 11 inch handouts about PROM that you can print and share with anyone you like! These beautiful flyers are perfect for placing in client folders, hanging at the nurse’s station, or giving out at maternity fairs.
To download the printer-friendly PDF and annotated bibliography for $0+ (suggested value $5), click HERE. (PayPal users, click here!) …
I’ve helpfully bolded the standard sales pitches. Hey, if it works for the Ginsu knife, why shouldn’t it work for the nonsense that Dekker is selling?
The key point: Dekker tries to monetize everything, no matter how trivial (“Those who give $25 will receive a high-resolution of these 8.5 by 11 inch PROM flyers”).
Dekker, a cardiology nurse, is trying to monetize a blog post about obstetrics, when the information is available anywhere for free.
Does anyone really pay for this crap?
2. The primary product being sold by the natural childbirth industry is distrust of obstetricians
Dekker disgorged a 10,000 word post on prelabor rupture of membranes that tells us nothing that we didn’t know decades ago, but you’d never know it by looking at the 24 point font, the exclamation points, and the charts and handouts.
Why? Because Dekker’s secondary purpose (after her primary purpose of enriching herself) is to encourage distrust of obstetricians.
There are many examples within the post, but the most egregious is probably the claim that obstetricians view prolonged rupture of membranes as an indication for C-section. Dekker trumpeted this claim several days ago on yet another outlet of the natural childbirth industry, ImprovingBirth.org.
When I questioned the provenance of this claim, I was offered a paper written back in 1966, not corroborated by any others and NEVER recommended by an obstetric organization. Shortly thereafter, my comments were deleted, I was banned from ImprovingBirth.org, and now I can’t find the post on their Facebook page.
Why? Presumably because I publicly pointed out the deliberately misleading attempt to portray obstetricians as incapable of following scientific evidence. Removing my comments and banning me is an indication that Dekker and ImprovingBirth.org are well aware that the claim is misleading. That didn’t stop Dekker from including it in her post:
Many doctors at this time said that women should give birth within 24 hours after their water broke, even if that requires a C-section.
In 1966, Shubeck et al wrote,
“With rupture of membranes, the clock of infection starts to tick; from this point on isolation and protection of the fetus from external microorganisms virtually ceases…Fetal mortality, largely due to infection, increases with the time from rupture of membranes to the onset of labor.” (Shubeck et al., 1966)
One doctor, Shubek, who no one listened to, back in 1966 said women should have a C-section if they hadn’t delivered within 24 hours is maliciously and misleadingly transformed into a policy that “many doctors” followed.
The entire point is gratuitous. No one really care what anyone said back in 1966, let alone someone that everyone else ignored, but Dekker couldn’t resist including it (and lying about it) because one of her primary purposes (after enriching herself) is to promote distrust of obstetricians.
3. Natural childbirth advocacy seeks to create personal conflict and hostility between women and their obstetricians
Dekker has learned nothing new. She has simply reiterated a policy that has been in place for at least 30 years, but you’d never know that. The implication of the piece is that Dekker has discovered something new, something ignored by obstetricians, and now is teaching women how to protect women from their ignorant doctors.
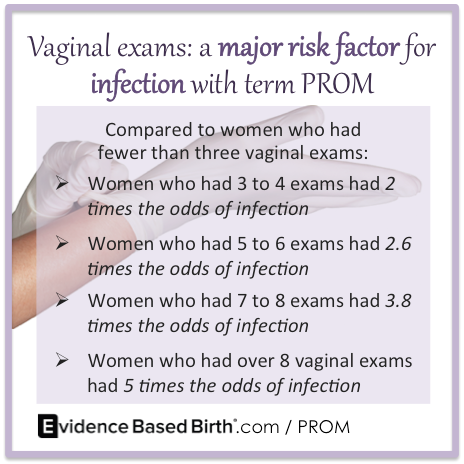
Dekker said everyone should feel free to use this image on their own blog, so I am doing so.
Dekker reiterates this in the Science and Sensibility piece:
Finally, probably the single most important thing that women need to know is to not let people put hands up your vagina after your water breaks! That is the single most important risk factor for infection, and hands need to be kept out as much as possible.
But who was recommending vaginal exams for prelabor rupture of membranes in the first place? No one.
What is the point of emphasizing to women that they should not let an obstetrician do what he or she wasn’t planning to do anyway? It’s like mentioning outdated procedures like shaves and enemas on a birth plan. It’s only purpose is to create conflict and mistrust between women and their providers.
Finally, Dekker’s piece, indeed her entire blog, is notable for one other feature characteristic of the natural childbirth industry. Dekker takes no responsibility for anything she writes. According to her disclaimer:
The Evidence Based Birth® website and blog content only provides general information that may or may not apply to your personal health condition or circumstances. The opinions expressed on this website and blog by Rebecca Dekker, PhD, RN, APRN or any other Evidence Based Birth® team members or volunteers on behalf of Evidence Based Birth® are strictly their own personal opinions and not the opinions or policies of any third party, including any health care provider, employer, educational or medical institution, professional association or charitable organization… (my emphasis)
If you rupture your membranes before labor begins, your obstetrician takes full responsibility for any advice, recommendations, examinations or procedures. Rebecca Dekker fills your head with misleading claims, implies that your obstetrician is not to be trusted and tells you what you should refuse and she takes no responsibility for any of that. Why? Because it’s just her personal opinion and if you are gullible enough to follow it, that’s your (and your baby’s) problem.
Thank you to Rebecca Dekker for publishing an plethora of words about nothing (and trying to make money from it) and for Science and Sensibility and Improving Birth.org for promoting it. All have helpfully illustrated the seductive marketing tactics of the natural childbirth industry.
They are in it for profit, not for your well being or your baby’s well being; natural childbirth advocacy is an industry and you should never forget it.